After a lifetime devoted to the care of women in Africa, Sr Dr Maura Lynch (UCD Medicine 1964) acquired the Ugandan name ‘Nakimuli’ meaning ‘Beautiful Flower’. She returned to Dublin to train as a surgeon after twenty years of missionary medical care in Angola. Returning to Africa, she established a centre of excellence in the treatment of obstetric fistula and for training of healthcare professionals at the Kitovu Healthcare Complex in St Joseph’s Hospital, Kitovu, approximately 140km from the Ugandan capital, Kampala.
Born in Youghal, Co. Cork on the 10th September 1938, Maura Lynch was the fourth of Patrick and Jane Lynch’s nine children. Due to her father’s work with An Post, the family lived at various times in Youghal, Carrick-on-Shannon, Killarney, Tralee and Limerick before finally settling in Dublin. After her secondary education, Maura joined the Medical Missionaries of Mary in Clonmel, Co. Tipperary in 1956. She enrolled in Medicine at UCD in 1958, graduating in 1964 in the top three of the class with an MB BCh BAO degree and a gold medal for surgery.
After completing her internship in medicine and surgery, she then went on to obtain a Diploma in Obstetrics and Gynaecology at the Royal College of Obstetrics and Gynaecology in London in 1966, followed by a Diploma in Tropical Medicine and Public Health in Lisbon in 1967. That same year she was assigned to the 200-bed Chiulo Mission Hospital in Angola where she acted as medical director sharing all the clinical work in medicine, surgery, obstetrics, gynaecology and paediatrics, TB and leprosy with another Sister Doctor for 20 years. During that time, she also worked as a lecturer and examiner in the Nurses Training School.
From 1983 to 1985, she studied for a post graduate fellowship in surgery in Ireland becoming an FRCSI from the Royal College of Surgeons of Ireland, England and Scotland. After her studies she returned to Angola. In 1987, she was assigned to Kitovu Mission Hospital in Uganda as a consultant surgeon/obstetrician/gynaecologist with responsibility for training of medical officers in surgical and obstetrics and gynaecology skills. That year she also spent three months in Nigeria training in obstetric fistula repair.
In the early 1990s, she was a co-founder member of the Association of Surgeons of East Africa (A.S.E.A) and in 1993 she initiated the Obstetric Fistula Repair programme inviting specialists from the UK to Kitovu three times a year to carry out 885 fistula repairs. During this time she also encouraged visiting surgeons and other consultants to come to Kitovu under the sponsorship of rotary Doctors Bank of Great Britain and Ireland. This provided consultant services as well as teaching and the passing on of skills to indigenous personnel.
Between 1999 and 2004, as interest and gradual awareness and appreciation of the dignity and needs of women in the developing world increased, there was greater recognition of the need for improved maternity services for the reduction and prevention of birth injuries. Between 2004 and 2005, Sr Dr Maura Lynch fundraised and supervised the building of a Fistula Unit in Kitovu with 28 beds. Over a 30 year career in Uganda, it is estimated that she was responsible for conducting over 1,000 vesicovaginal fistula repairs, which Professor Bill Powderly, former Dean of Medicine at the UCD School of Medicine described as,
An astonishing record that one can confidently say will never be bettered…. As a result of seeing at first hand the physical, psychological and social isolation endured by African women, she became a champion of dignity and justice for women in the developing world.
In 2007, she was awarded an Honorary Fellowship by the UCD Medicine and Medical Sciences in recognition of her 43 years of medical care in Africa. In 2009, she was nominated by UNFPA (Uganda) as ‘Leader in fight against Fistula’ and this was followed in 2013 with an honorary Fellowship in Obstetrics and Gynaecology from London College of Obstetric & Gynaecology (FR.C.O.G). In 2015 Sr Maura was awarded the prestigious Council of Europe’s North-South Prize. She was chosen in recognition of her ground-breaking work with women whose lives have been devastated by obstetric fistula in Sub-Saharan Africa. She was nominated for the award by Irish Ambassador Anne Webster and it was presented to her by the President of the Portuguese Republic, Professor Cavaco Silva, in the Portuguese Parliament. The North-South Prize of the Council of Europe is awarded every year to two personalities, one from the North and the other from the South. The prize rewards their commitment to the defense and promotion of human rights, democracy and the rule of law as well as to the development of intercultural dialogue and the reinforcement of the North-South partnership and solidarity.
She died unexpectedly in Kampala Hospital on 9th December 2017, on the day scheduled for a golden jubilee celebration of her life in Africa. Speaking at her funeral, the representative of the Irish Ambassador to Uganda, Ms Áine Doody noted,
Sr Maura was a woman of faith. In terms of the characters of Martha and Mary in the new testament story Sr Maura was more Martha than Mary with her life being about a tremendous amount of doing for others. She was a member of the Medical Missionaries of Mary that was founded in the 1930’s in Drogheda. This band of women have served generously and heroically in a good number of developing world countries. She was a proud member of this great congregation of women.
Alongside her well recognized achievements what stands out in the life of Sr Maura was her energy, generosity, outgoing personality and sense of fun. At the Irish Embassy hosted lunch in Kampala each year for the Irish Missionaries on the day of the St Patrick’s Day reception Sr Maura was the life and soul of the party. She was the one to dance and encourage others to do so and enjoyed a song and the craic.
Throughout her distinguished medical career, Sr Dr Maura Lynch was a pioneer of innovative surgery and surgical training, a champion of impoverished women’s health services in Africa and a missionary who dedicate herself to the service of others.
Ar dheis Dé go raibh a h-anam dílis
Professor Owen Smith, UCD Professor of Paediatric and Adolescent Medicine and Consultant Paediatric Haematologist at Our Lady’s Children’s Hospital, Crumlin, is part of an international team that has made a breakthrough in juvenile myelomonocytic leukaemia (JMML).
The study, published in Nature Communications, shows for the first time, that JMML can be broken into three subgroups with unique molecular and clinical characteristics, through analysis of DNA methylation. Based on high, intermediate or low methylation, differences in the underlying mutations, and significantly, in the prognosis of the disease have been identified. High methylation is associated with a poor clinical outcome, low methylation with a good outcome.
JMML is an aggressive myeloproliferative cancer of early childhood characterized by mutations activating RAS signaling. Without adequate treatment, survival for most children with JMML is less than 1 year. Treatment involves stem cell transplantation, and even with this, the 5 year event-free survival still reaches only about 50%. Current established clinical and genetic markers do not differentiate the clinical and biological heterogeneity of this disease.
This study is a huge advance in the care of children with this type of cancer; providing a method to predict the disease outcome, and to stratify risk of relapse. From this, future work in the mechanisms underlying the DNA methylation in this disease, will potentially lead to new avenues of treatment.
The research is supported by the National Children’s Research Centre at Our Lady’s Children’s Hospital Crumlin.
RAS-pathway mutation patterns define epigenetic subclasses in juvenile myelomonocytic leukemia.
Lipka DB, Witte T, Toth R, Yang J, Wiesenfarth M, Nöllke P, Fischer A, Brocks D, Gu Z, Park J, Strahm B, Wlodarski M, Yoshimi A, Claus R, Lübbert M, Busch H, Boerries M, Hartmann M, Schönung M, Kilik U, Langstein J, Wierzbinska JA, Pabst C, Garg S, Catalá A, De Moerloose B, Dworzak M, Hasle H, Locatelli F, Masetti R, Schmugge M, Smith O, Stary J, Ussowicz M, van den Heuvel-Eibrink MM, Assenov Y, Schlesner M, Niemeyer C, Flotho C, Plass C.
Nat Commun. 2017 Dec 19;8(1):2126. doi: 10.1038/s41467-017-02177-w. PMID: 29259247
Adapted from an Article by the National Children's Research Centre.
We are delighted to announce that the Summer Student Research Awards (SSRA) Programme 2018 is open again for project submission.
Proposals are sought for eight-week laboratory, clinical, patient-centred or educational research projects, to be undertaken by our undergraduate students within the College of Health and Agricultural Sciences and College of Engineering and Architecture during Summer 2018.
If your project has ethical approval, or is exempt from full ethics review, we ask that you upload a copy of the relevant approval letter to our new online form. If you do not think your project requires ethical approval, or exemption from full review, there is an option on the form for you to select. However, we will ask you to state why you think this is the case (for example, the intended project might involve a student reviewing data that is already in the public domain).These measures were put in place to assist us all in complying with the mandatory ethics requirements for UCD undergraduate students undertaking research as part of their degree programmes.
Investigators at the National Maternity Hospital have commenced enrolment of neonates into an European paediatric clinical study to investigate if prophylactic oropharyngeal surfactant at birth can reduce the rate of endotracheal intubation for respiratory failure within 120 hours of birth.
The Paediatric Clinical Research Infrastructure Network (PedCRIN) was founded in response to the widely acknowledged difficulties in conducting investigator-led trials of investigational medicinal products in children. PedCRIN brings together the European Clinical Research Infrastructure Network (ECRIN) and the founding partners of the European Paediatric Clinical Trial Research Infrastructure (EPCT-RI) and is funded by the European Union’s Horizon 2020 programme.
Launched in January 2017, PedCRIN is a four year project which aims to develop capacity for the management of multi-national paediatric non-commercial clinical trials. PedCRIN seeks to effectively bridge paediatricians and other partners across and beyond Europe to combine resources and expertise to conduct, manage and execute robust studies, whilst mininising risk and protecting the child participants.
In February 2017, PedCRIN invited applications for funding for investigator-led multi-country paediatric or neonatal clinical studies on medicine products trials that would be conducted in Europe. Three awards were made from 13 applications from six coordinating countries, Ireland, France, Norway, Italy, Germany and the UK.
Prof Colm O’Donnell (UCD Full Clinical Professor and consultant neonatologist at the National Maternity Hospital, Holles Street was among one of the successful applicant groups. The group secured funding of €430,000 from PedCRIN to support the POPART (Prophylactic Oropharyngeal Surfactant for Preterm infant: A Randomised Trial) trial. The POPART trial which commenced in June 2017 will determine whether, among infants born before 29 weeks of gestation, does prophylactic oropharyngeal surfactant at birth compared to no intervention, reduce the rate of endotracheal intubation for respiratory failure within 120 hours of birth?
This trial will enrol 250 infants in several European countries (Ireland, Sweden, Norway, Denmark, Czech Republic, Italy, Portugal). Recruitment started at the National Maternity Hospital in Dublin in mid-December 2017 and to date 5 babies have been enrolled at the Dublin maternity hospital. The trial is sponsored by UCD and forms the central part of current PhD research by Dr. Madeleine Murphy, a Clinical Research Fellow funded by the National Children’s Research Centre.
More information: http://www.ecrin.org/projects/pedcrin/call-outcome
The UCD Radiography and Diagnostic Imaging Group invites applications to its new online Professional Diploma in Early Pregnancy and Gynaecological Ultrasound. Closing date for applications to the next intake is Friday 5th January 2018.
The programme adds to the Group’s extensive portfolio of ultrasound and speciality imaging programmes that support maternal and fetal health. With the exception of two introductory study days at UCD’s Belfield Campus, the twelve month programme is delivered entirely online to accommodate those with a busy clinical schedule or who work across the country.
The programmes is aimed at obstetric and gynaecological trainees at Senior House Officer, Registrar, Specialist Registrar or Senior Registrar level, consultants specialising in obstetrics and gynaecology, with approval to practice in Ireland; midwives registered with An Bord Altranais or the UKCC, who provide antenatal care; or Radiographers with the approval to practice Radiography in Ireland or Northern Ireland, who currently practice ultrasound. Other professionals are considered on individual merit (eg general nurses or general practitioners), but must be actively scanning in order to undertake modules in the Graduate Certificate Programme.
To undertake this programme, participants must be actively scanning in an obstetric/gynaecological ultrasound department and have a named clinical supervisor. Students must arrange a clinical placement and provide evidence of an agreement to spend a minimum of 160 hours practicing clinical obstetric and gynaecological ultrasound while undertaking the two modules necessary to complete the Diploma.
It is recommended that participants spend as much time as possible performing clinical ultrasound examinations while undertaking ultrasound modules. Students will maximise their potential to develop high level clinical and academic skills in ultrasound by exceeding the minimum clinical hours stated for each module. Applicants should be computer literate and have continuous internet access for the duration of this programme.
Participants must provide written evidence of an agreement with an obstetric/gynaecological ultrasound department to provide clinical ultrasound experience and supervision throughout the programme. This agreement must be signed by the named clinical supervisor.
Programme Pathways
The Diploma comprises two modules (RDGY41000 Early Pregnancy Ultrasound and RDGY41150 Gynaecological Ultrasound). Following completion of the Diploma, there is an option to progress to the Graduate Certificate Obstetric Ultrasound by taking a third module (Fetal Biometry, Liquor and Placenta). In order to do this the Diploma graduates will be required to apply to the Grad Cert programme and apply for Recognition of Prior Learning for the 2 modules already completed.
The Professional Diploma programme offers an exit strategy, if required, whereby a student can exit the programme with a 10 credit Professional Certificate in Early Pregnancy Ultrasound.
How to Apply
Further information on the programme can be found here. To apply for the programme, please use the University online application system (www.ucd.ie/apply).
International applicants should contact the academic programme director for a full list of entry requirements. Information on studying at UCD as international students is available here.
Academic Programme Coordinator
Dr Mary Moran
Lecturer/Assistant Professor UCD Radiography and Diagnostic Imaging, UCD School of Medicine, UCD Health Sciences Centre University College Dublin, Belfield, Dublin 4.The UCD School of Medicine offers an extensive portfolio of over fifty graduate taught programmes ranging from Professional and Graduate Certificate through to Diploma and Master’s Degree level across a range of biomedical and clinical specialties.
Our programmes are delivered by academic experts in their fields with extensive clinical experience and by clinical staff drawn from our extensive adjunct faculty.
Our programmes are designed to support continuous professional development of healthcare staff as well as provide specialist education to a generalist audience including those working in healthcare support roles.
Our programmes are delivered on a full-time, part-time or on an occasional basis at our Belfield campus, at our specialist clinical training sites, and in some instances, online to accommodate those with busy clinical service commitments. Programmes typically commence with a September and/or a January intake.
To explore our Graduate Taught Programme Portfolio further, please see http://www.ucd.ie/medicine/studywithus/
To apply for a programme, please see www.ucd.ie/apply
Wed, 3 January 18 13:02
The UCD School of Medicine offers an extensive portfolio of over fifty graduate taught programmes ranging from Professional and Graduate Certificate through to Diploma and Master’s Degree level across a range of biomedical and clinical specialties.
Our programmes are delivered by academic experts in their fields with extensive clinical experience and by clinical staff drawn from our extensive adjunct faculty.
Our programmes are designed to support continuous professional development of healthcare staff as well as provide specialist education to a generalist audience including those working in healthcare support roles.
Our programmes are delivered on a full-time, part-time or on an occasional basis at our Belfield campus, at our specialist clinical training sites, and in some instances, online to accommodate those with busy clinical service commitments. Programmes typically commence with a September and/or a January intake.
Specialist graduate training is available in
With multiple entry and exit points as well as a series of common module components, our programme portfolio allows you to design your continuous professional development around your career needs. As research-intensive Medical School within Ireland’s global University, our graduate taught programmes also offer an opportunity to undertake research projects leading to MD, MCh, MAO, MSc and PhD degree awards.
To explore our Graduate Taught Programme Portfolio further, please see http://www.ucd.ie/medicine/studywithus/
To apply for a programme, please see www.ucd.ie/apply
The UCD School of Medicine offers an extensive portfolio of over fifty graduate taught programmes ranging from Professional and Graduate Certificate through to Diploma and Master’s Degree level across a range of biomedical and clinical specialties.
Our programmes are delivered by academic experts in their fields with extensive clinical experience and by clinical staff drawn from our extensive adjunct faculty.
Our programmes are designed to support further continuous professional development of healthcare professional as well as provide specialist education to a generalist audience including those working in healthcare support roles.
Our programmes are delivered on a full-time, part-time or on an occasional basis at our Belfield campus, at our specialist clinical training sites, and in some instances, online to accommodate those with busy clinical service commitments. Programmes typically commence with a September and/or a January intake.
Specialist graduate training is available in
With multiple entry and exit points as well as a series of common module components, our programme portfolio allows you to design your continuous professional development around your career needs. As research-intensive Medical School within Ireland’s global University, our graduate taught programmes also offer an opportunity to undertake research projects leading to MD, MCh, MAO, MSc and PhD degree awards.
To explore our Graduate Taught Programme Portfolio further, please see http://www.ucd.ie/medicine/studywithus/
To apply for a programme, please see www.ucd.ie/apply
Applications are now invited for Medical Traineeships in Human Anatomy at the UCD School of Medicine commencing September 2018 for the 2018/2019 Academic Year.
The research focus in Human Anatomy at UCD currently involves but is not limited to:
Upcoming projects include:
Medical Traineeships in Human Anatomy
A number of MD and PhD Scholarships are offered with Research MSc and MCh also available. The full-time scholarship programme is available to EU students only offering an €18,000 taxfree stipend along with payment of 75% of student EU fees. Scholarships are reviewed on an annual basis and may be extended based on satisfactory progression in teaching and research.
Successful candidates will undertake a graduate research degree while gaining skills and experience teaching functional and clinical anatomy to medical and allied health students. Strong academic skills and competency in Anatomy are desirable as part of the selection criteria, along with proficient communication skills. Prior clinical training is desirable but not a mandatory requirement.
More information on this course, see www.ucd.ie/medicine/anatomy
Closing Date: Friday 9th March 2018 (5pm)
Mucus plugs are a plausible mechanism of chronic obstruction in severe asthma, and EPO-generated oxidants may mediate mucus plug formation. That was the conclusion of a clinical study reported recently in the Journal of Clinical Investigations by a multi-institutional collaboration led by the University of California, San Francisco. Lead author in the study was Dr Eleanor Dunican, now consultant respiratory physician at St Vincent’s University Hospital and Associate Professor at the UCD School of Medicine.
Asthma is a complex and heterogeneous condition with multiple underlying inflammatory and structural airflow abnormalities that lead to symptomatic disease. Researchers have sought to develop methods to characterise different asthma types with a view to developing personalise, targeted therapies. Dr Dunican and colleagues developed a non-invasive method of measuring airway mucus accumulation in asthma using multi-detector computed tomography. Using this imaging technique, the group were able to demonstrate a reproducible ‘mucus score’ and established that mucus plugging was common among patients with severe asthma. Subjects with high mucus scores had more severe airflow obstruction and higher indices of eosinophilic airway inflammation.
The clinical evaluation of this methodology involved 146 subjects with asthma and 22 controls and analysed the relationship between mucus plug scores, forced expiratory volume in 1 second (FEV1) and airway eosinophils. The researchers also used airway mucus gel models to examine if oxidants generated by eosinophil peroxidase (EPO) promoted mucus plug formation by oxidising cysteine thiol moieties.
Mucus plugs occurred in at least 1 of 20 lung segments in 58% of subjects with asthma and in only 4.5% of controls and the plugs in patients with asthma persisted in the same segment for many years. A high mucus score (plugs in 4 or more segments) occurred in 67% of cases with FEV1 of less than 60% of predicted volume, 19% with FEV1 of 60-80% and 6% of subjects with FEV1 greater than 80%. High mucus score was also associated with marked increases in sputum eosinophils and EPO. EPO catalysed oxidation of thiocyanate and bromide by hydrogen peroxide in vitro to generate oxidants that crossline cysteine thiol groups and stiffen thiolated hydrogels.
In an accompanying commentary in the same journal, Steven Georas of the University of Rochester Medical Centre noted that
the development of the radiographic mucus score represents an elegant example of translational research that will further our understanding of asthma heterogeneity.
He observed that while the study had shown association between high mucus scores and airflow obstruction, it is difficult to know if this association is causal. Future longitudinal studies might provide some insight into whether high mucus scores precede the development of airflow obstruction in at-risk subjects. It is hoped that non-invasive radiographic methods such as that described here will help clinicians define specific asthma sub-sets and assist in the evaluation of targeted therapies.
Mucus plugs in patients with asthma linked to eosinophilia and airflow obstruction.
Dunican EM, Elicker BM, Gierada DS, Nagle SK, Schiebler ML, Newell JD, Raymond WW, Lachowicz-Scroggins ME, Di Maio S, Hoffman EA, Castro M, Fain SB, Jarjour NN, Israel E, Levy BD, Erzurum SC, Wenzel SE, Meyers DA, Bleecker ER, Phillips BR, Mauger DT, Gordon ED, Woodruff PG, Peters MC, Fahy JV; National Heart Lung and Blood Institute (NHLBI) Severe Asthma Research Program (SARP).
J Clin Invest. 2018 Feb 5. pii: 95693. doi: 10.1172/JCI95693. [Epub ahead of print] PMID: 29400693
All plugged up - noninvasive mucus score to assess airway dysfunction in asthma.
Georas SN. J Clin Invest. 2018 Feb 5. pii: 99726. doi: 10.1172/JCI99726. PMID: 29400694
President of Ireland, Michael D. Higgins, honoured the recipients of the SFI President of Ireland Future Research Leaders Award at a special ceremony in Áras an Uachtaráin. Five awards by Science Foundation Ireland, representing a €7 million investment, will also support the additional recruitment of 15 research positions. Research supported by the awards will examine novel drug targeting for the treatment of multiple sclerosis and obesity-related diseases, regenerative medicine, immunology, tissue engineering, protein engineering, and memory storage in amnesia.
A passionate political voice, poet and academic, President Higgins has been a long-standing advocate of inclusive citizenship and creativity, highlighting not only the positive contribution of science to society, but also the links between the creativity of artists and the innovation of scientists. Equally, the President has stressed the importance of placing scientific research in a clear social, cultural and ethical context, saying that the benefits of scientific advances should be spread as widely as possible.
The awardees of the SFI President of Ireland Future Research Leaders Award are Dr Tomás Ryan, who was recruited from Massachusetts Institute of Technology (MIT) to Trinity College Dublin (TCD); also based in TCD is Dr Lydia Lynch, recruited from Harvard University, USA; Dr Claire McCoy was recruited from the Hudson Institute of Medical Research, Melbourne, Australia to the Royal College of Surgeons (RCSI); Prof John Laffey has been recruited from St Michael's Hospital, Toronto, Canada to the National University of Ireland Galway (NUI Galway); and Dr Christina Kiel has been recruited from the Centre de Regulació Genòmica (CRG), Barcelona, to University College Dublin (UCD).
Congratulating the awardees, Prof Mark Ferguson, Director General of Science Foundation Ireland and Chief Scientific Adviser to the Government of Ireland, said
The President of Ireland Future Research Leaders Award is designed to attract to Ireland outstanding new and emerging research talent. In supporting these talented and innovative individuals, we are delighted to recognise early career researchers who have already displayed exceptional leadership potential at the frontiers of knowledge. The development of leadership skills in these researchers early in their careers is vital to ensure research and innovation in Ireland continues to progress. Our investment highlights the importance that Science Foundation Ireland places on supporting all stages of academic careers, and on the attraction and retention of star researchers.
Our investment highlights the importance that Science Foundation Ireland places on supporting all stages of academic careers, and on the attraction and retention of star researchers"
Dr Christina Kiel's research focuses on the structural analysis of signalling pathways and protein interaction networks relevant in human diseases, such as colon cancer and retinal degenerations. The senior investigator at UCD Systems Biology Ireland said
I am delighted to receive this award, which will enable me to recruit an interdisciplinary team of experimental and computational scientists to understand cellular signalling networks in colorectal cancer. The award will support my research in the field of cell signalling and protein engineering. The research will identify the network connections that are deranged by genetic mutation and then aim to exploit this aberrant connectivity to destroy cancer cells. Ultimately, this approach may provide better mechanism-driven diagnostics and treatments.
Prof Carel Le Roux (UCD Professor of Experimental Pathology) describes in layperson's terms the results of clinical research trial comparing semaglutide with dulaglutide (when administered with metformin) in the treatment of people with Type 2 diabetes.
This summary informs study participants and the public about a research study (called a ‘clinical trial’). Results of research studies about medicines are described in a report. It is for researchers, health professionals and for people who approve medicines. This is a summary of that report.
Thank you to the participants and site staff who made this study possible.
When and where did the study take place?
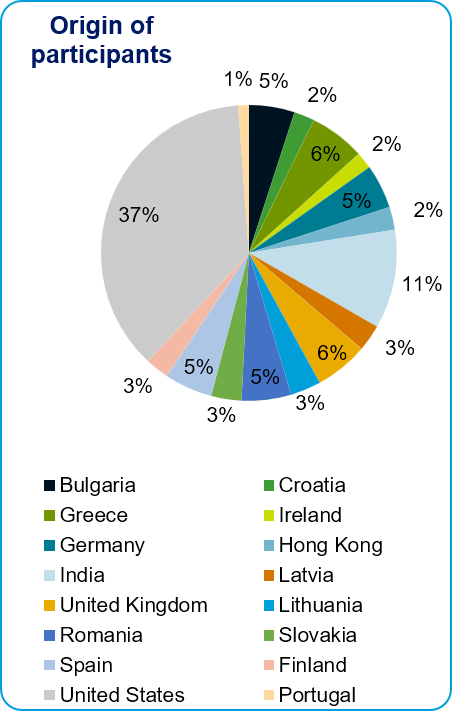
The study took place from January 2016 to May 2017 in the following countries: Bulgaria, Croatia, Finland, Germany, Greece, Hong Kong, India, Ireland, Latvia, Lithuania, Portugal, Romania, Slovakia, Spain, United Kingdom and United States. The study went as planned.
Why is this study important?
People with type 2 diabetes (T2D) have high levels of sugar in their blood. This is because their insulin does not work properly. Insulin is a hormone that helps control the amount of sugar in the blood. High blood sugar can be harmful to the body, and especially to the heart.
To treat T2D, medicines help the body lower blood sugar. There are many different treatments to help lower blood sugar.
This was a phase 3 study, meaning that it was done in a large group of people worldwide.
In this study, researchers compared the new treatment (semaglutide) with another once-weekly treatment in the same class (dulaglutide) used for T2D.
What did researchers want to know?
Researchers wanted to know more about semaglutide in treating people with T2D.
They wanted to compare how semaglutide and dulaglutide worked on blood sugar.
In this study, 1199 participants with T2D took part. All participants were taking metformin. Metformin is a medicine to help lower blood sugar. All participants had high sugar levels, and had their HbA1c measured. HbA1c is a measure of the blood sugar (levels) over the last 3 months.
People could not take part if they had

About the study medicines
This study compared 2 medicines of a class of drugs called GLP-1-RAs. These medicines are a changed form of the human GLP-1 made in the body. GLP-1 is a hormone made in the gut. It helps the body release more insulin. Insulin helps to control blood sugar.
The study medicines were semaglutide and dulaglutide.
Semaglutide and dulaglutide are used in the US, and dulaglutide in Europe to help treat T2D.
The study medicines were taken by an injection pen. The medicine was injected with a needle under the skin.
Participants got study medicine once a week for 40 weeks.
About the study
The study participants were split into 4 groups by chance. 2 groups got semaglutide and 2 groups got dulaglutide. The participants and researchers knew what study medicine they got.
Each group got a different amount (dose) of study medicine.
Researchers compared groups 1 and 2 to each other. Researchers compared groups 3 and 4 to each other.
In this study researchers saw an improvement (lowering) in blood sugar levels with the majority of participants. The blood sugar levels were lower in participants who got semaglutide compared to dulaglutide, which was seen after 40 weeks with study medicine. Researchers looked at HbA1c. This is a blood test that shows how well blood sugar is being controlled. The mean HbA1c values at the end of the study are listed below
The participants in group 1 had lower HbA1c than in group 2. The participants in group 3 had lower HbA1c than in group 4.
These are the results from this study. Other studies may show something different.
What are side effects?
Side effects are unwanted medical events thought by the doctor to be caused by the medicines in the study.
A side effect is serious if it:
Not all participants in this study had side effects.
What serious side effects did the participants have?
6 of 601 participants (1%) had serious side effects after taking semaglutide.
Serious side effects were:
Each of these happened in 1 of 601 (less than 1%) participants taking semaglutide.
3 of 598 participants (1%) had serious side effects after taking dulaglutide.
Serious side effects were:
Each of these happened in 1 of 598 (less than 1%) participants taking dulaglutide.
The participants taking semaglutide had a similar amount of serious side effects to those taking dulaglutide.
What were the most common side effects?
The most common side effects that affected more than 1 of 10 participants were:
feeling sick in the stomach (nausea)
loose stools (diarrhoea)
Other common side effects were:
throwing up (vomiting)
not feeling hungry
high levels of lipase in blood
This study is part of a programme that includes many final and planned studies. This is to find out how semaglutide should be used to treat people with T2D. This was only one study; other studies may show different results.
Findings from this study will be used to further improve the optimal use of semaglutide.
Studies with semaglutide are still going on and more studies are planned.
Details on these studies can be found on the websites listed in Section 10.
Study name: Efficacy and safety of semaglutide versus dulaglutide as add-on to metformin in subjects with type 2 diabetes
Phase of clinical development: phase 3b
EudraCT number: 2014-005375-91
UTN number: U1111-1164-8495
National Clinical Trial number: NCT02648204
IND number: 79,754
Research sponsor: Novo Nordisk A/S
Contact details of Sponsor: Novo Nordisk A/S, Novo Allé, 2880 Bagsvaerd, Denmark
Tel: +45 4444 8888
E-mail: clinicaltrials@novonordisk.com
Internet: www.novonordisk.com
You can find more information about the study at these websites:
For general information about clinical studies please go to: www.novonordisk-trials.com/website/content/about-clinical-trials.aspx
Novo Nordisk | Trial ID: NN9535-4216 | This document includes known facts as of the time the document was finalised.

The 2018 UCD Medicine Clinical Commencement ‘White Coat’ Ceremony took place in UCD O’Reilly Hall on Friday 9th February 2018. A key milestone for our medical students, the ceremony marks the formal transition from a predominantly classroom-based education to full immersion into clinical training at our hospital site and in the community.
The proceedings were led by Dean of Medicine and Head of School, Professor Patrick Murray supported by a selection of our academic and clinical faculty. Students from the Stage 4 direct entry undergraduate and stage 2 graduate entry medicine took part in the ceremony which was attended by many friends and family. As part of the ceremony, students are ‘robed’ with white coats by faculty members as an important symbol of their transition into the role of doctor in training.
In opening the ceremony, Prof Murray noted,
Before addressing your transition to the clinical environment, it is important to recognise that today is equally a recognition of the extensive knowledge of biomedical science that you have mastered to date, under the tutelage of our expert faculty (several of whom are on stage tonight), which puts you in a position to apply this knowledge of the scientific basis of health and disease in the clinical arena. In UCD, we think it is important to mark this transition formally, and this tangible marker of career progression is very much appreciated by students and family members alike.
The School takes this opportunity to remind students of the privilege but also the attendant responsibilities which come with the next stage of their education and training.
The awarding of a white coat is both practical and symbolic; in addition to protection of clothing, the white coat represents the increased professional privileges, but also the responsibilities that accompany this transition. In addition to meeting the expectations for professionalism in your practice, conduct, and ethics, you are also joining a medical community in which it is a doctor’s primary responsibility to be a strong advocate for their patients, above all other considerations (personal and otherwise). This is particularly important in a period of shrinking healthcare resources, in which you must reinforce the standard of evidence-based best practice to guide management of patients under your care. The latter also mandates development of leadership and teamwork skills, which we will also seek to develop before your graduation and beyond. Finally, it is important that your behaviour in the clinical setting is geared toward protecting patients and optimizing their outcomes, whether it’s by rigorous hand hygiene, up to date vaccination against communicable diseases, or other aspects of evidence-based clinical practice.
added Professor Murray.
Prof Murray asked for a moment of silence to remember recently deceased classmate, Ms Ruth Potter.
It is with profound sadness that I remember the untimely passing of your classmate Ruth Potter, in late November of last year. In Limerick at her funeral, I saw first-hand how she was valued as a classmate and friend to many of you. I also know that your presence there in Limerick was a great comfort to her family. Others in the UCD School of Medicine community have suffered recent bereavements of family and friends. For these reasons, we in the School are always conscious that your early clinical exposures may stir up difficult emotions. Please share your burden with us, and we will provide you whatever supports you need.
The keynote address was given by Professor Ronan O’Connell, UCD Emeritus Professor of Surgery and consultant colorectal surgeon at St Vincent’s University Hospital. In his introduction, Prof Murray congratulated Professor O’Connell on being recently elected Vice President of the Royal College of Surgeons in Ireland. Professor O’Connell compared and contrasted his clinical experience with that which awaits our students as they commence their clinical careers.
My generation was fortunate to experience the third Industrial Revolution, the one that introduced digital technology, the internet and mobile computing. You, on the other hand, as you begin your professional lives, you do so at the birth at the fourth industrial revolution, in which artificial intelligence, robots, nanotechnology, quantum computing and biotechnology will change everything in ways that you cannot even imagine…. So I see your greatest challenge not as lacked of access to knowledge or diagnostic facilities but resource management in an era of personalized and very expensive treatment and the ever-increasing costs of managing chronic disability.
Both Professor O’Connell and Professor Murray recognised the daunting transition ahead of our students and highlighted the peer support available from clinical colleagues. Prof Murray noted,
To help you in what can be a stressful transition, you will have the guidance of your supervising medical colleagues, in what is truly a clinical apprenticeship. You will find that the consultants, GPs, and house staff you work with are an overwhelmingly bright, hardworking, dedicated group of professional experts who advocate for their patients every day. You will also work in interdisciplinary teams, another change for many, and you will learn to work with groups of equally professional and dedicated colleagues in other health care disciplines, who similarly have much to teach you. Please be assured that in this challenging period, you will have the support of your peers, medical colleagues, and university counsellors.
The white coat is a very symbolic representation of the medical profession. Historically it portrayed the authority of the physician and is generally regarded as a sign of professionalism. It also symbolises the responsibilities that define the practice of medicine, and particularly the responsibility of doctors to put the interests of their patients first. This responsibility is an obligation that commences as a medical student and continues throughout one’s medical career. In his address, Prof O’Connell took up this theme of professionalism and the patient/doctor relationship.
Always remember your relationship with the patient is a privileged one. One that depends on the patient's trust in your professionalism. Professionalism is above all else about respect, dignity and trust. You respect the patient's dignity and they trust in your knowledge and your care.
We would like to take this opportunity to thank our students, their families and friends and all the faculty and staff who participated in the ceremony. The proceedings were broadcast live on our websteam to enable families of our overseas students witness this key milestone. A high resolution video recording and a selection of photographs are available on our YouTube and Flickr channels respectively.
Resources
Prof Patrick Murray’s Opening Address [180209 - Prof Murray Address at WCC2018]
Prof Ronan O’Connell Keynote Address [180228 - Address by Prof Ronan O'Connell, Clinical Commencement 2018]
Photographs from the UCD Medicine Clinical Commencement ‘White Coat’ Ceremony [here]

The School is pleased to announce a new research programme focus on improving survival rates of children and teens affected by cancers of the blood. With funding from the National Children's Research Centre and CMRF Crumlin, the School has been able to establish the Brendan McGonnell UCD Professor of Paediatric Molecular Haematol-Oncology and has appointed Prof Jonathan Bond to this position,
The result of an innovative partnership between the three organisations, this new professorship has been developed to advance research into paediatric and adolescent cancers of the blood, with the aim of improving survival rates for those affected.
The new Chair is supported, under the NCRC Research Leadership Award Scheme, by a significant legacy donation from the late Mr Brendan McGonnell to CMRF Crumlin.
The NCRC Research Leadership Award Scheme aims to build research capacity in key areas of child health, and this new Chair at UCD will play a pivotal role in the development of a molecular and translational research programme into childhood blood cancers.
said Dr Jacinta Kelly, Chief Executive of the NCRC.
Child and young adolescent haematological cancers account for approximately 40% of all cancers in children up to the age of 16. Professor Bond’s research programme, which will be carried out at Systems Biology Ireland, UCD, will focus on understanding how normal gene regulation is subverted in acute leukaemia with the ultimate goal of developing new and better treatments for every child and adolescent with this blood cancer.
Professor Owen Smith CBE, Professor of Paediatric and Adolescent Medicine said,
We are sincerely grateful to the NCRC and CMRF for their commitment to further research into paediatric blood cancers at University College Dublin which is a truly fitting gesture in memory of Brendan McGonnell and his extraordinary philanthropy.
We are delighted to welcome Professor Bond to the University, where he will be a significant asset to our research activities in paediatric haemato-oncology. His appointment will have a major impact in the field of paediatric cancer in Ireland and internationally.
Professor Jonathan Bond, Brendan McGonnell UCD Professor of Paediatric Molecular Haemato-Oncology said,
I am very grateful that NCRC, CMRF Crumlin and UCD have used Brendan McGonnell’s generous donation to create this position. This is a hugely exciting opportunity to perform research that will improve the treatment of children with blood cancers.”
Lisa-Nicole Dunne, CEO, CMRF Crumlin, said,
We are delighted to be able to support this incredible work with the NCRC. Paediatric cancer is one of the research areas we are proud to fund at CMRF Crumlin. We receive no governmental funding, so legacies left by the likes of Brendan McGonnell really have a wonderful, lasting impact on the treatments available for future generations of sick children.
Professor Bond has relocated to Ireland following the completion of a research fellowship at the Hôpital Necker-Enfants Malades, Paris. He completed his undergraduate medical study at Trinity College Dublin and trained as a clinical paediatric haematologist in Ireland before obtaining a PhD in Molecular Haematology at the MRC Clinical Sciences Centre (now the London Institute of Medical Sciences) and Imperial College London.
The National Children’s Research Centre (NCRC) is over 50 years old and was the first dedicated research centre on the site of an Irish hospital. Today, it offers state of the art research laboratories, research funding through competitive grant calls, and a children’s clinical research unit at Our Lady’s Children’s Hospital, Crumlin, where clinical trials and studies take place. Together, these facilities allow the NCRC to support full bench to bedside research for children. It has been funded by charitable donations to CMRF, Crumlin, since its inception. www.nationalchildrensresearchcentre.ie/
CMRF Crumlin (the Children’s Medical Research Foundation) was established in 1965 and is the principal fundraising body for Our Lady’s Children’s Hospital, Crumlin and The National Children’s Research Centre. We drive fundraising to allow for research into the cause, treatment, care and prevention of children’s illness and disease and to actively support excellence in the care and treatment of sick children by providing additional equipment, facilities and assistance to patients and their families within Children’s Hospital at Crumlin. www.cmrf.org
The late Brendan McGonnell was a successful business man, philanthropist, vintage car enthusiast and patron of the arts. Born in Dublin in 1944, a pupil of CBS Synge Street, his kindness and thoughtfulness for sick children and the disadvantaged in our society was evident by the many worthy causes he supported throughout his life. He developed Heathers, a Swedish-style country lodge in Glencree Valley complete with a Children's Village. Following his death in 2014, he made bequests to various Irish charity groups including the Children's Medical Research Foundation.
Fri, 30 March 18 13:51
There have been many false dawns heralding an era of personalised medicine but for one young patient, work by Genomics Medicine Ireland and researchers within the UCD Academic Centre on Rare Diseases has particular significance allowing her speak for the first time in four years.
Mary-Ann Cleary is a young patient with Progressive Dystonia, a very rare disease in children that causes painful seizing of the muscles. Her condition had progressed so severely that she was unable to move or speak, eventually resulting in her being admitted to the Intensive Care Unit. After researchers identified her as a suitable candidate for Deep Brain Stimulation (DBS) treatment, she underwent the procedure with dramatic results. She has uttered her first word in four years, “Mama”, following treatment.
Genomics Medicine Ireland (GMI), together with the UCD Academic Centre on Rare Diseases (ACoRD), worked with Professor Mary King, UCD Full Clinical Professor and Consultant Paediatric Neurologist and Research Fellow Dr Eva Forman at Temple Street Children’s Hospital to follow genomic sequencing that identified a mutation in gene KMT2B.

This was shown to respond to a treatment called Deep Brain Stimulation (DBS), a procedure that is not typically performed on young children. In September 2017 Mary-Ann underwent DBS, and in November she spoke for the first time in four years. Today she is able to move around, speak, laugh, and play.
This case offers insight into the potential in genomics for precision medical diagnostics and treatments. Previously UK, where the family now lives, were unable to identify a successful treatment for the patient, despite a series of tests over several years which all ultimately proved inconclusive. However, after taking genomic analysis of the patient’s blood sample by GMI, it took only weeks to process, which was a fraction of the time and cost relative to what had been undertaken and which resulted in a far more efficient and effective resolution.
Professor Mary King said,
We are delighted that Mary-Ann could be treated so successfully and so quickly thanks to genomics. This new cutting-edge field can significantly reduce the patient journey, which for complicated or rare diseases can currently involve a number of lengthy, invasive tests, followed by a course of treatments which may have varying effectiveness.
Seán Ennis, Chief Scientific Officer and co-founder of Genomics Medicine Ireland and Director of UCD ACoRD, commented:
Genomic research studies usually take many years to yield significant actionable results, so to achieve such an important, tangible outcome so quickly is amazing, especially given the critical condition and time-sensitive nature of the patient. This example has really shown the true potential of genomics, which is accurate, targeted, quick and affordable diagnostics and treatment; it’s a real win-win for all involved.
Genomics Medicine Ireland is currently undertaking research into Multiple Sclerosis, Inflammatory Bowel Disease, and Brain Tumours in conjunction with hospitals across Ireland and the company also recently announced they will be examining Alzheimer’s disease.
Established in 2013, the UCD Academic Centre on Rare Diseases is focused on the study of rare genetic diseases, with a view to the identification of the mutation(s) causing the disease. Once a causal mutation(s) is established, the objective is to develop diagnostic tests for translation back into a clinical setting. Once a gene is implicated, our PIs work to further investigate the gene function and biological pathways involved in the condition. The ultimate aim is to investigate those conditions / genes which might be amenable to drug targeting or gene therapy.

The UCD Perinatal Research Centre based at the National Maternity Hospital, Holles Street was launched today with a symposium highlighting maternal and fetal health research undertaken over the past ten years and a reflection on the future challenges of the global obesity epidemic on mother and child health.
Led by Professor Fionnuala McAuliffe, UCD Full Professor of Obstetrics & Gynaecology at National Maternity Hospital, the Centre aims to coordinate national and international collaborative research in maternal and fetal health, including diabetes and nutrition in pregnancy, to improve the long-term health of mothers and their infants. Professor McAuliffe is an internationally recognised expert in pregnancy, maternal and fetal health, diabetes and nutrition in pregnancy.
Among the research studies being carried out at the Centre is the Pregnancy Exercise and Nutrition Study with Smartphone Application Support (PEARS), which involves over 500 women. Women with a BMI of greater than 25 kg/m2 have a higher risk of developing gestational diabetes and a low glycaemic index (GI) diet in pregnancy has been shown to lower glucose intolerance. The PEARS study was designed to assess the impact of a lifestyle intervention package, consisting of a low GI diet and an exercise programme, with support provided by a smart phone app, on the incidence of gestational diabetes in an overweight and obese pregnant population.
Professor Fionnuala McAuliffe said,
“I am delighted to announce the launch of the UCD Perinatal Research Centre. The overall aim of our research activities is to enable women to have the healthies pregnancies, and the healthiest babies, they can.
The PEARS study is a great example of the work which will be carried out at the Centre and the findings of this study will be published shortly. The initial results have found that this intervention package reduced the incidence of babies born large, for gestational age, which is an extremely exciting finding. The novel addition of a specifically designed smart phone app holds considerable potential to alter maternal behaviour in a positive way.”

Speaking at the launch, Professor Orla Feely, UCD Vice-President for Research, Innovation and Impact said,
“I welcome the launch of the new UCD Perinatal Research Centre and I wish Professor McAuliffe and her innovative research team every success in the future. The research which will be carried out at this Centre will have far-reaching impact in improving the long-term health of mothers and their infants, not only in Ireland but around the world.”
Professor Mary Day, CEO, Ireland East Hospital Group, said,
“The impact of UCD Perinatal Research Centre will further the ambition of the Ireland East Hospital Group, in partnership with UCD, to develop as an academic health science centre which will harness the expertise location with our tertiary hospitals and UCD to address the current and further challenges addressing our population. This opportunity will deliver greater access for patients to leading edge research, translating into improved patient benefits.”
Other studies taking place at the UCD Perinatal Research Centre include the ROLO Kids and ROLO PreTeen studies. These are longitudinal follow-up studies of the ROLO study, involving 800 pregnant women, which assessed the impact of a low GI diet on birth weight, maternal glucose intolerance and gestational weight gain. Children from the ROLO study have been followed up, along with their mothers, at 6 month, 2 years, and 5 years of age, with the 10 year follow-up to start shortly, in order to determine whether maternal nutrition and low GI diet in pregnancy impacts on maternal and child health in the long term.
The research within the UCD Perinatal Research Centre is funded by grants from Health Research Board Ireland, Science Foundation Ireland, the European Union, and the National Maternity Hospital Medical Fund.
 (1).jpg)
There are fine lines in surgery where life and death decisions have to be made at the end of a scalpel. The James B. Coakley Medal for Dissection in honour of a former Professor of Anatomy at UCD is awarded for the best dissection of a given body part.
James B. Coakley was Professor of Anatomy and Head of the Department of Human Anatomy at University College Dublin from 1962 – 1988. To honour his distinguished career and dedication to anatomy teaching, the James B. Coakley Medal for Dissection was established. This is prestigious award that will provide a small select number of students a privileged opportunity to work with a precious educational resource.
Applications are now invited for the James B. Coakley Medal for Dissection 2018.
James B. Coakley Medal for Dissection 2018 Application Form
Completed application forms should be returned to Mr. Steven Masterton, Room C209, UCD Health Sciences Centre. Only one entry per candidate is permitted.
Dissections will be undertaken from Tuesday 3rd July (start date) to Thursday 23rd August (end date).
Steven Masterton
Award Administrator
T: +353 1 716 6344
Closing Date Tuesday 1st May 2018 (5pm)
Roche Newman Fellowship in Neurology
As part of its programme to provide postdoctoral research opportunities for scholars of proven academic excellence, University College Dublin is pleased to announce the Roche Newman Fellowship in Neurology.
The Roche Newman Fellowship in Neurology will be based at St Vincent’s University Hospital’s Department of Neurology, under the principal supervision of Dr Christopher McGuigan. The Department has over thirty years of research history in this area and has published extensively in international peer reviewed journals.
The research project will focus largely on the biomarkers to monitor progressive forms of Multiple Sclerosis in Ireland.
The successful candidate will have at least one year’s experience of Neurology at a specialist registrar level. The Newman Fellow will have a significant clinical role in the Department and will be expected to complete an MD thesis (optional extension to PhD). The Roche Newman Fellowship in Neurology is tenable for two years.
Informal enquires regarding this Fellowship may be directed to Dr. Christopher McGuigan: c.mcguigan@ucd.ie.
A completed Newman Fellowship Application Form 2017, a copy of your CV and two copies of the Newman Fellowship Referee Form should be returned to:
Dr. Meadhbh O’Halloran
UCD Graduate Studies
UCD Research
Tierney Building
Belfield, Dublin 4
T: 01 716 4047
E: graduatestudies@ucd.ie
The closing date for receipt of completed applications is 30th April 2018.
Aristotle held that the heart was the seat of intelligence until Herophilos, one of the founders of Anatomy, showed it to be the brain. While many may see Anatomy as being a largely discovered field there is still much we can learn from the human form.
The research focus in Human Anatomy at UCD currently involves:
The one year (or possible extension for the duration of research degree) full-time scholarship programme offers an €18,000 tax-free stipend along with payment of 100% of student EU fees. Scholarships are reviewed on an annual basis and may be extended based on satisfactory progression in teaching and research. Successful candidates will undertake a graduate research degree while gaining skills and experience teaching functional and clinical anatomy to medical and allied health students. Strong academic skills and competency in Anatomy are desirable as part of the selection criteria, along with proficient communication skills. Prior clinical training is desirable but not a mandatory requirement.
Monday 7th May 2018 (5pm)
More information on this course here
Researchers around the world capture and share proteogenomics data to further understand the global diversity of people and cancers in unique populations.
Precision medicine is an approach that allows doctors to understand how a patient's genetic profile may cause cancer to grow and spread, leading to a more personalized treatment strategy based on molecular characterization of a person's tumor. However, precision medicine as a genomics-based approach does not yet apply to all patients because genetic mutations do not always lead to changes of the corresponding proteins. Therefore, integrating genomics and proteomics data, or proteogenomics, presents as a new approach that may help make precision medicine a more effective treatment option for patients.
In the latest publication of the journal Cell, Dr. Henry Rodriguez, Director of the Office of Cancer Clinical Proteomics Research, and colleague Prof Stephen Pennington, UCD Professor of Proteomics, detail the evolution of precision medicine, and how the National Cancer Institute is taking key strides to coordinate with the international cancer research community to provide an integrated, open-data approach to precision oncology. These efforts allow researchers to work together and streamline research efforts, troubleshoot issues, standardize protocols and workflows, and share progress to address the challenges and advance precision medicine efforts.
Ms Sharon Omiwole, Stage 1 Medicine student, has been named the winner of FameLab Ireland – the national science communication competition for students.
FameLab helps emerging scientists and engineers to acquire valuable skills to communicate their work to a non-scientific audience. The competition is organised by the British Council Ireland and funded through Science Foundation Ireland’s Discover programme.
Sharon will go on to represent Ireland at the international finals of the competition at the Cheltenham Science Festival in the UK. She was selected by a judging panel of nine science communicators at the sixth FameLab Ireland national finals at the Science Gallery Dublin.
Each contestant delivered a three-minute talk that was judged according to content, clarity and charisma. During her 180 seconds, Sharon won the judges over with her talk entitled ‘Willy Wonka and the Coffee Factory’. It outlined in detail the effects of caffeine and its associated hormones and chemicals – adrenaline and dopamine.
Sharon is a first-year medical student at UCD with a keen interest in science. She credits her father, a doctor, for inspiring her to pursue medicine. She dedicates her spare time to volunteering in clinics, retirement homes, day-care and homeless shelters.
Margie McCarthy, Interim Director, Innovation and Education Directorate, Science Foundation Ireland, said SFI aims to encourage more people to engage with STEM through its Discover Programme.
“FameLab helps realise that aim by offering participants the opportunity to gain vital skills in communicating what can be complex research topics in an engaging way, inspiring others to join the conversation,” she said.
The winners from all participating countries will compete in June at the international finals at the Cheltenham Science Festival in the UK.
FameLab is an initiative of the Cheltenham Festivals. It is managed by the British Council Ireland in collaboration with Newstalk 106-108fm, NUI Galway, Science Gallery Dublin, Trinity College Dublin, University College Cork, University College Dublin, University of Limerick and a range of science research centres.
The British Council is the UK’s international organisation for cultural relations and educational opportunities and it has a presence in over 100 countries including Ireland.
Original article by: Jamie Deasy, digital journalist, UCD University Relations

Prof Kenneth Wolfe, Professor of Genomic Evolution has been awarded a European Research Council Advanced Grant for the second time in his career. He is the first ever Ireland-based researcher to receive two of the highly sought after research funding awards.
ERC Advanced Grants fund well-established research leaders with internationally renowned track records. They support transformative, high-risk research projects at the frontiers of science and scholarship. They are part of the EU's Research and Innovation programme, Horizon 2020.
Professor Wolfe, UCD School of Medicine and UCD Conway Institute, is one of three researchers in Ireland to receive an ERC Advanced Grant in the recent call. He will receive €2.37m for his new project called: Killer plasmids as drivers of genetic code changes during yeast evolution.
Professor Wolfe’s project will examine the evolution of genetic code and the changes it underwent in several species of yeast. The genetic code is the set of instructions used by living cells to translate information encoded in DNA into proteins. It is universal in most living organisms, but in the yeast species Professor Wolfe is investigating, the code was translated differently. He will test a new hypothesis that the genetic changes were caused by a deadly toxin.
“I am delighted to congratulate Ken on this very prestigious and highly competitive award,” said Professor Orla Feely, UCD Vice-President for Research, Innovation and Impact. “Following on from his election as a Fellow of the Royal Society in 2017, this reinforces Ken’s position as one of the leading scientists in his area worldwide.”
Professor Wolfe studies how genomes and chromosomes are organised and how they came to have the structures they have today. His group discovered that the genomes of many species became completely duplicated during their evolution, doubling the number of genes they contain.
He was one of the first Principal Investigators supported when Science Foundation Ireland was established in 2001, and was awarded his first European Research Council Advanced Grant in 2011. He is a former President of the Society for Molecular Biology and Evolution, and a Member of the Royal Irish Academy.
He is one of five Fellows in Ireland of the Royal Society. Professor Wolfe is the first scientist to be elected to the Royal Society from University College Dublin since Edward Conway in 1947.
Professor Fergal O'Brien, Department of Anatomy at the Royal College of Surgeons in Ireland and The Thomas Mitchell Professor of Cognitive Neuroscience at Trinity College Dublin, Professor Rhodri Cusack, also received the grants in this call.
Original article by: Jamie Deasy, digital journalist, UCD University Relations
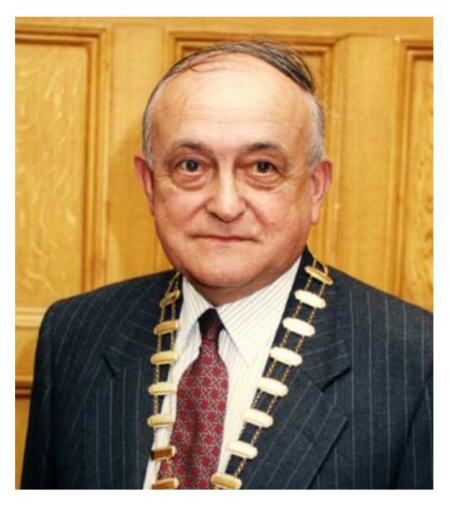
The death has been announced of Professor Edward Guiney (UCD MB BCh BAO 1956, MCh 1961), a distinguished alumnus who had a stellar career as an internationally recognised paediatric surgeon, researcher and teacher.
Commenting on the passing of his former colleague, UCD Professor of Paediatrics, Professor Brendan Drumm noted,
Eddie Guiney had a great intellect, qualifying at the top of the class in UCD. He was a man of remarkable humility whose focus in life was on contributing to the betterment of society. He was a skilled paediatric surgeon who treated sick children and their families with such genuine kindness and caring. Wisdom and generosity of spirit are attributes that I will always associate with Eddie and I was privileged to benefit from these through his advice and constant encouragement.
We offer our condolences to Professor Guiney’s family and friends, former colleagues and patients.
Ar dheis Dé go raibh a anam
By way of tribute, we reproduce an interview with Professor Guiney recorded on the occasion of his retirement in 2011 which was first published in the Royal College of Surgeons in Ireland’s News Scope publication. Reproduced with the kind permission of RCSI.
Originally published in RCSI, News Scope, September 2011, Issue 3.
In Barry O’Donnell’s book ‘Irish Surgeons and Surgery in the Twentieth Century’, Professor Edward Guiney is described as a ‘quick, superb technical surgeon, who showed great humanity in dealing with patients and parents’ and also as ‘a prodigious worker’. It is probably these characteristics that led Professor Guiney to have such a successful career as a Paediatric surgeon.
Professor Guiney was born in 1931 in Dublin and educated at Belvedere College before going on to study medicine in University College Dublin and graduating in 1956. Eddie spent his postgraduate years working at St. Vincent’s Hospital in Dublin before moving to the Regional Hospital Galway in 1957 for two years where he was a senior house officer and registrar. In 1958 he moved back to Dublin as senior registrar and tutor in surgery in St. Vincent’s Hospital, completing a Master of Surgery (MCh) degree in 1961. Having been awarded a two-year travelling Fellowship in surgery by the NUI, Professor Guiney went to St Thomas’s Hospital in London between 1960 – 1961 as a lecturer in surgery and following that as a Research Fellow in Massachusetts General Hospital and Harvard Medical School.
Upon his return from the United States, Eddie lectured in surgery in UCD until 1965. It was around this time that Prof Guiney decided to move into paediatric surgery. From 1965 to 1966 he worked as a senior surgical registrar in the Alder Hey Children’s Hospital in Liverpool before returning to Dublin as a consultant paediatric surgeon in Our Lady’s Hospital for Sick Children and Temple Street Hospital (1966 – 1997) and the National Children’s Hospital, Harcourt Street (1970 – 1997), often working a one-on-one rota in his hospital appointments.
Throughout his entire career, Eddie was actively involved in research, culminating in his appointment as Director of Research at the Children’s Research Centre in 1976 a post he held until 1989. While in St. Thomas’s he was involved in work on the lymphatic system and at Massachusetts General, he was involved in transplantation biology. In Dublin, he was concerned with liver surgery and transplantation. He led an experimental liver transplant surgery at the UCD Research Centre, which resulted in the survival of a number of pigs, one of which gave birth to fourteen piglets. As you can no doubt imagine, in 1972 this was a world first and led to his involvement in the national liver transplant programme at St. Vincent’s Hospital, Dublin. His other clinical interest during his career was in the management of children with Spina Bifida and Hydrocephalus.
When asked to reflect on his career, Prof Guiney recalls Joe McMullen as having a large influence on his career progression. ‘I had a lot of respect and admiration for him and he is probably the one surgeon that really stands out for me,’ Prof Guiney said. Working as a surgeon, he said ‘was a great career, very satisfying and I feel very privileged with what comes from such a career.’
Prof Guiney is firm believer in the importance of post-operative care and communication. ‘Aside from obviously the technical aspect of being a surgeon, post-operative care and communication are essential, especially when it comes to working with children. Communication with parents is essential. When you have a child as a patient, you actually have three patients; the mother, the father and the child itself.
When asked whether it was hard to work with children, Prof Guiney said that it is a question he gets asked a lot but ‘it’s not hard, as long as you’re properly trained. Children have their own way of communicating and you just have to learn this.’
Prof Guiney was elected as President of the British Association of Paediatric Surgeons. His election as President against a strong London candidate was a tremendous personal achievement for Eddie and it mirrored the esteem in which he was held. He also served as President of the Society for Research in Spina Bifida and Hydrocephalus and of the Irish Paediatric Association.
Unfortunately in 2006 Eddie’s wife Sheila passed away. They had three children, Eddie, Michael and Carina. Eddie is the award-winning film producer and co-founder of Element Pictures. Michael is a Consultant Radiologist in St James’s Hospital and the Beacon Hospital and Carina lives in Belfast and has two children. He was an avid reader and a keen sports spectator. After his retirement, Professor Guiney continued to work as a Surgeon Prosector in RCSI up to 2014, following on from his role as RCSI Professor of Paediatric Surgery (1991 – 1997) and later Professor Emeritus at the College.
Adapted from an article courtesy of RCSI originally published in RCSI News Scope, September 2011. Photo credit: Irish Surgeons and Surgery in the Twentieth Century, B.O’Donnell

The University has announced the appointment of Prof Desmond J Tobin as new Director of the UCD Charles Institute of Dermatology and Professor of Dermatological Sciences. Prof Tobin, currently Professor of Cellular Biology and Director of the Centre for Skin Sciences at University of Bradford, will take up his appointment from 1st September 2018.
A native of Co. Meath, his undergraduate studies in immunology at Maynooth University and NESCOT (Surrey, GB) were followed by PhD studies in 1991 on the presumptive autoimmune disorder alopecia areata at St. John’s Institute of Dermatology, University of London. Two years postdoctoral training at the Department of Dermatology, New York University Medical School were followed by his appointment as Assistant Research Professor of Dermatology (1993-1996). He has a Postgraduate Diploma in Management from the Chartered Management Institute (London).
Des holds/held fellowships from the Royal College of Pathologists (FRCPath), Royal Society of Biology, Higher Education Academy, and Institute of Trichologists. He serves as vice-president of the Institute of Trichologists, and is President of the British Society for Investigative Dermatology. He is a member of the British Association of Dermatologists Research Committee, and member of the advisory board of the UK-TREND.
Prof. Tobin’s research has focused predominantly, but not exclusively, on pigmentation of the skin and hair in health and disease, immune-mediated hair follicle disorders, and hair follicle growth. His research has been recognized with the John Pawelek Lectureship (ASPCR) and F John G Ebling lectureship (EHRS), among others. His research program has received funding from a mixed portfolio of Industry, Government, and Charity sources etc. Des has published over 200 articles, with a current H-Index of 56 (Scopus). He is editor of the Henry Stewart Talks Collection – ‘Skin Biology’ series.
We look forward to welcoming Des as Director of the UCD Charles Institute of Dermatology and to the UCD School of Medicine where he will also hold the post of UCD Professor of Dermatological Sciences.
Launched in 2008, the UCD Charles Institute is Ireland's first academic institute dedicated to dermatology research and education. The Institute’s vision is to become a world leader in dermatology research and training, which will lead to improved patient care through the discovery of new treatments and therapies. UCD Charles Institute actively partners with leading companies serving the skin health and care market to deliver specific research and innovation objectives. Using a multidisciplinary, systems biology approach, the Institute research team are working to uncover key drivers of skin disease and ageing. This approach is leading to exciting new innovations for the management of skin ageing and treatment of serious skin disease. [more]
The School was delighted to welcome back our alumni to the 2018 UCD Medical Graduates Association Alumni Reunion which took place on Friday, 11th May 2018. Now firmly established as a key highlight of the School calendar, the event was attended by graduates from the Medicine Classes of 1958, 1963, 1968, 1978, 1988, 1993, 1998, 2008 and 2017.
The alumni celebrations included a series of presentations from class representatives followed by tours of the UCD Health Science Centre and UCD Charles Institute. The event concluded with a Gala Dinner in the Conrad Hotel, Earlsfort Terrace at which the Medical Graduates Association Distinguished Graduate Award was presented to our Dean and Head of School, Professor Patrick Murray (UCD Class of 1988).
The series of presentations by alumni was chaired by Professor Fionnuala McAuliffe, President of UCD MGA and UCD Professor of Obstetrics & Gynaecology at the National Maternity Hospital and Professor Patrick Murray, Dean of Medicine and Head, UCD School of Medicine. In his introduction, Prof Murray acknowledged how the School’s reputation is forged by the successful careers and leadership of our graduates across the globe. He paid tribute to the strong tradition of mentorship and support which preceding classes offer to our current students and highlighted international research elective opportunities.

Presenters at Alumni Reunion 2018
Attendees also took the opportunity to participate in tours of the UCD Health Sciences Centre which has been home to the Medical School since 2006 and the UCD Charles Institute of Dermatology. Many of those present were delighted to see again the historic Kevin Barry Memorial Window by Richard King of Harry Clarke Stained Glass Studio. This artwork was commission by classmates of Irish rebel Kevin Barry, a first year UCD medical student who was executed at the age of 18 for his part in the War of Independence. First unveiled in 1934 by President of Ireland, Eamonn de Valera in the School’s original Earlsfort Terrace home, the window was relocated in 2011 to UCD Belfield.
Over 260 guests attended a reunion dinner at the Conrad Hotel, Earlsfort Terrace at which the 2018 UCD Medical Graduates Association Distinguished Graduate Award was presented to Professor Patrick Murray (UCD Medicine Class of 1988). The citation was ready by classmate and friend, Dr Eoin Bergin, consultant nephrologist at the Midland Regional Hospital, Tullamore. Dr Bergin described Prof Murray’s distinguished career as a clinician, researcher and as Dean of Medicine, noting that Prof Murray is board-certified in the USA in four clinical specialties (internal medicine, nephrology, critical care medicine and clinical pharmacology). He highlighted Prof Murray's leadership as a student, a young doctor in training and throughout his academic career culminating in his recent strong leadership of the UCD School of Medicine. The Distinguished Graduate Award was presented to Prof Murray by his School colleague, Prof Fionnuala McAuliffe, President of the UCD Medical Graduates Association.

Prof Fionnuala McAuliffe and Dr Eoin Bergin presenting UCD MGA Distinguished Graduate Award to Prof Patrick Murray.
A selection of photographs from the 2018 Reunion can be found here.
Following such a highly successful event, the School will shortly commence planning for the 2019 Alumni Reunion which will feature the classes of 1959, 1964, 1969, 1979, 1984, 1994, 1999, 2009 and 2019.
An international clinical trial involving researchers at Our Lady’s Children’s Hospital Crumlin has demonstrated that extended use of all-trans retinoic acid coupled to risk-adapted consolidation can achieve high remission rates in childhood acute promyelocytic leukaemia whilst limiting anthracycline exposure. The clinical trial which was co-authored by Professor Owen Smith, UCD Full Professor of Paediatric and Adolescent Haematology, was published recently in the American Society of Hematology’s Blood publication.
Pediatric acute promyelocytic leukaemia (APL), a rare childhood neoplasm, can be cured with all-trans retinoic acid (ATRA) and anthracycline. However, most published trials to date have employed high cumulative doses of anthracyclines. The investigators report the outcome of patients with newly diagnosed APL enrolled into the International Consortium for Childhood APL (ICC-APL-01) trial, which reduced anthracycline exposure but extended that of ATRA.
The study recruited 258 children/adolescents with molecularly/cytogenetically-proven APL. Patients were stratified into standard-risk (SR) and high-risk (HR) according to the baseline WBC count (< or ≥10x109/L); both groups received identical induction treatment with ATRA (25 mg/m2/day, for 30 consecutive days) and 3 doses of idarubicin (12 mg/m2/dose). Two or three blocks of consolidation therapy were administered to SR and HR patients, respectively, while maintenance therapy with low-dose chemotherapy and ATRA cycles was given to all patients for 2 years. The cumulative dose of daunorubicin-equivalent anthracyclines in SR and HR patients was lower than that of previous studies, being 355 mg/m2 and 405 mg/m2 in SR and HR patients, respectively.
Hematologic remission was obtained in 97% of patients; 8 children died of intracranial hemorrhage in the first 2 weeks following diagnosis. The 5-year overall and event-free survival for the whole cohort were 94.6% and 79.9%, respectively; they were 98.4% and 89.4% in SR and 84.3% and 74.2% in HR patients (p=0.002 and p=0.043, respectively).
These data demonstrate that extended use of ATRA coupled to a risk-adapted consolidation can achieve high cure rates in childhood APL and limit anthracycline exposure. The trial was registered at www.clinicaltrials.gov with the following identification number EudractCT 2008-002311-40.
Risk-adapted treatment of acute promyelocytic leukemia: results from International Consortium for Childhood APL
Reproduced with Prof Smith’s kind permission.

Picture: (l-r) Prof Gerard Fealy, Dean of Nursing and Head of School, UCD School of Nursing, Midwifery & Health Systems; Dr Sally Ann Lynch, Consultant Clinical Geneticist in OLCHC; Prof Eileen Treacy, Clinical lead, National Clinical Programme for Rare Diseases; Prof Thilo Kroll, Professor of Health Systems Management and HRB PPI Ignite Lead for UCD, UCD School of Nursing, Midwifery & Health Systems; Prof Orla Feely, UCD Vice-President for Research, Innovation and Impact; Ms Kay Duggan-Walls; Health Research Board and National Contact Point for Health; Dr Suja Somanadhan, Assistant Professor of Children’s Nursing, UCD School of Nursing, Midwifery & Health Systems; Dr Avril Keenan, CEO, MRCG, Mr Philip Watt, CEO, Cystic Fibrosis Ireland; Mr Paul Harkin, Director of Strategic Development, UCD School of Medicine; Dr Sean Ennis, Director of UCD Academic Centre on Rare Diseases.
UCD hosted its annual Rare Disease Symposium on 3rd May 2018 which aimed to highlight developments in rare disease research and education, to raise public awareness of rare diseases and build a more cohesive University-wide collaboration in partnership with patient adovcate organisations.
Originally scheduled to take place in March on International Rare Disease Day 2018, the event was postponed due to the unseasonal weather conditions which included a snow storm. The symposium was conjointly hosted by the UCD Schools of Medicine, and Nursing, Midwifery and Health Systems, the UCD Academic Centre on Rare Diseases, along with Rare Disease Ireland, the Medical Research Charities Group (MRCG), and the Irish Platform for Patient Organisations (IPPOSI).
The audience of almost 200 attendees included people living with a rare disease, families, researchers, policymakers and students, who gathered to discuss the symposium's main themes of 'Innovative Approaches to Rare Diseases' and 'Holistic Care in Rare Diseases'.
In welcoming the delegates, Professor Orla Feely, UCD Vice President for Research Impact and Innovation, spoke of the importance of healthcare professionals and support groups for parents and families coming together to shae research, progress and ideas. Professor Eileen Tracey, Clinical Lead, National Clinical Programme for Rare Diseases and UCD Full Clinical Professor, discussed progress on rare diseases at both national and European levels. Dr Sean Ennis, Director of the UCD Academic Centre on Rare Diseases, updated the audience on ongoing research into rare diseases and highlighted the impact of research on better patient managment leading to improved healthcare for patients living with rare diseases in Ireland and across the globe.
Dr Avril Kennan, Chief Executive Officer of the Medical Research Charities Group chaired a panel discussion on 'Innovative Approachs to Rare Diseases' featuring
Ms Raquel Castro, Head of Social Policy at EURORDIS, a non-governmental patient-driven alliance of patient organisations across Europe, gave a video presentation on 'Social Care in Rare Diseases, reporting on the INNOVA Care Project. Ms Julie Power, Vasculitis Ireland gave a powerful testimony on the lessons for and impact of patient-led advocacy.
Dr Aoife Brinkley, Senior Clinical Psychologist at the National Centre for Inherited Metabolic Disorders led a second panel discussion on the theme of 'Nothing about us with out us - Holistic Care' featuring:
Dr Paula Byrne, Associate Professor at the UCD School of Medicine chaired a session featuring reflections by UCD students on their experiences with and exposure to rare diseases during the education. We thank both Ms Kate Bailey (UCD Medicine) and Mr John Hutchings (UCD Nursing) for their excellent and impactful presentations.
The final session focused on research funding and research support opportunities respectively with presentations by Ms Kay Duggan-Walls (Health Research Board EU Programmes Officer & National Contact Point for Health, Horizons 2020) and Dr Anne-Louise Holloway (Research Programme Officer, National Programmes, UCD Research & Innovation).
Dr Derick Mitchell, Chief Executive Officer of the Irish Platform for Patient Organisations, Science and Industry, drew the meeting to a close, summarising the key lesson and themes which had emerged throughout the symposium before a musical performance by Ms Alison Sweeney, who runs a music therapy service at the National Children's Hospital in Tallaght.
The School would like to sincerely thank Dr Suja Somanadhan and her organising committee on an excellent and informative symposium and to thank the many patient advocates who participated throughout the event.

The University has announced Professor Michael Keane as the next Dean of Medicine and Head of UCD School of Medicine for a five-year term from the 1st September 2018. Prof Keane succeeds Prof Patrick Murray who completes his five-year term at the end of this academic year.
Professor Keane is a consultant respiratory physician and is currently UCD Professor of Medicine and Therapeutics at St Vincent’s University Hospital where he is also Clinical Director and where he has been acting Chief Executive Officer. The Hospital has recently announced the appointment of Ms Kay Connolly as Hospital Chief Executive Officer.
Prof Keane graduate from UCD School of Medicine in 1989 and following his initial clinical training in Dublin, moved to the university of Michigan, Ann Arbor where he undertook a fellowship in pulmonary and critical care medicine in 1995. He subsequently took up a faculty position at the University of Michigan in 1998 and in 2000 moved to the University of California, Los Angeles where he was Professor of Medicine and Programme Director for the UCLA Interstitial Lung Disease Center.
Professor Keane returned to UCD and St Vincent’s University Hospital in 2007 when he was appointed Professor of Medicine and Therapeutics and consultant respiratory physician. He established a Science Foundation Ireland-funded research group at the UCD Conway Institute and became Lead Clinical Coordinator for Lung Cancer Services within the St Vincent’s Healthcare Group.
His research interests include the biology of idiopathic pulmonary fibrosis including the mechanisms and mediators involved in the pathogenesis of the disease. Current research studies include the function and regulation of the IL-13 receptors, regulation of fibrocytes differentiation and the potential of mesenchymal cells to attenuate fibrosis. His research group has a particular interest in animal models of fibrosis.
Professor Keane has over 130 peer-review publications and has presented extensively at international conferences. He has been Associate Editor of the Journal of Immunology and on the Editorial Board of the American Journal of Respiratory and Critical Care Medicine, He is a member of the American Thoracic Society, the American College of Chest Physicians, the American Association of Immunology, Society of Critical Care Medicine and a Fellow of the American College of Chest Physicians.
At St Vincent’s University Hospital, Professor Keane has been a member of the Hospital’s Medical Executive which he has also chaired and has been Lead Clinical Director for a number of years. He has been acting Chief Executive Officer since 2015. He is a founding member and director of Dublin Academic Medical Centre and has played a lead role in the establishment of the Ireland East Hospital Group.
We wish Professor Keane well in his appointment and look forward to working with him as Dean of Medicine and Head of School over the next five years.
Mindreading is an initiative that explores the overlaps between physical and mental health, and specifically:
It also examines the impact of their work on clinicians and compassion fatigue or burnout of clinicians, which are very topical in health services today. This conference builds on the first conference held at University College Dublin in March 2017, and a 6-week long installation in the dlr Lexicon library, Dún Laoghaire last year. Several patient groups are involved from Ireland and the UK in Mindreading 2018 which takes place between 18th and 19th June 2018 in Birmingham, England. Participants at the conference will include poets, clinicians, literature and medical humanities experts, and experts by experience.
Themes to be addressed during Mindreading 2018 include:
Much literature deals with the impact of illness on friendships and social supports. Of course, illness does not exist in a vacuum. Prof Sally Shuttleworth (University of Oxford) will discuss the ideas of "Fractured lives" in literature and how this reflects social change.
In his workshop on "The Pariah Syndrome: Why Do So Many People Desert the Ill?" Dr Neil Vickers (King’s College London) examines what a variety of scientific disciplines have to tell us about the isolation of the ill and their loved ones. Among the disciplines to be covered will be neuroscience, infant research and attachment studies.
Returning for this year's conference following a hugely successful workshop at the UCD/ Lexicon in 2017, the College of Psychiatrists of Ireland and the REFOCUS user group return with their popular workshop exploring stigma experiences in mental health.
In a session on Narrative, Culture, and Public Health, Prof Christopher Fitzpatrick (UCD School of Medicine), Professor Gerardine Meaney, Dr Cormac O’Brien, and Dr Clare Hayes-Brady (all from UCD School of English, Drama and Film) will discuss the use of Poetry and Applied Drama in Clinical Practice. Prof Meaney will talk about her project Contagion, Biopolitics, and Migration in European Cultural Memory and Dr Cormac O'Brien will discuss his work on communities of care in Irish culture in the HIV/AIDS crisis.
This has been the subject of much debate in recent weeks and gaps in services are identified in much media coverage in the UK and Ireland. Prof Dame Sue Bailey OBE DBE (Professor of Child Mental Health at the University of Central Lancashire) will give a keynote address. Prof Dame Bailey was appointed an Officer of the Order of the British Empire (OBE) in 2002 for services to Mental Health and young offenders and in 2013 was promoted to Dame Commander of the Order of the British Empire (DBE) for services to Psychiatry and for voluntary service to People with Mental Health Conditions. She was President of the Royal College of Psychiatrists from 2011 to 2014. Prof Dame Baily is currently Senior Clinical Advisor for Mental Health and Learning Disability for Health Education England, and Chair of the Children and Young People’s Mental Health Coalition. Her research interests include development of needs and risk assessment measures for use with young offenders with mental illness and development of community and secure inpatient treatment for young offenders both nationally and internationally.
A panel of speakers from Action on Postpartum Psychosis (APP), the national UK charity for women and families affected by Postpartum Psychosis, will speak about their experiences of mental illness, coping with a new-born baby, and the therapeutic value of writing.
There will also be a keynote address by Prof Chris Fitzpatrick entitled 'What I learned from Sylvia Plath, Ingmar Bergman and Kieran O'Driscoll'. Prof Fitzpatrick is a Consultant Obstetrician & Gynaecologist, and former Master/CEO, Coombe Women & Infants University Hospital and UCD Clinical Professor at the UCD School of Medicine. He is the lead clinician for the Royal College of Physicians of Ireland’s programme Bereavement in the Maternity Services: An Approach to Caring and Coping - Parents and Clinicians - developed in association with patient advocacy groups and the Abbey Theatre, Ireland’s national theatre.
There is much attention at present paid to burnout among doctors and clinicians, and to times when the health service gets things wrong.
Prof Brendan Drumm, Professor of Paediatrics at the UCD School of Medicine and the inaugural Chief Executive Officer of the Irish Health Services Executive, will explore the theme of ‘Using narrative to promote the responsibility and the privilege of caring’ in a keynote address. Assoc. Prof Elizabeth Barrett (Consultant in Child and Adolescent Psychiatry at the Children’s University Hospital and Associate Professor at the UCD School of Medicine) and Dr Katherine Furman (Lecturer in Philosophy at Department of Philosophy, University College Cork) will explore clinician burnout and compassion fatigue in her presentation entitled "From Greek Tragedy to Twitter: Understanding Doctors’ Vulnerability".
MIND READING 2018
THE ROLE OF NARRATIVE IN PHYSICAL AND MENTAL HEALTH AND THE EXPERIENCE OF ILLNESS
18th-19th June 2018
University of Birmingham
Speakers Include: Dame Professor Sue Bailey, Professor Femi Oyebode, Professor Sally Shuttleworth, Professor Brendan Drumm, Professor Chris Fitzpatrick, Associate Professor Elizabeth Barrett, Dr Neil Vickers, and Dr Melissa Dickson
Do clinicians and patients speak the same language? How might we bridge the evident gaps in communication? How can we use narrative to foster clinical relationships? Or to care for the carers? How does illness impact upon our sense of self?
This two-day programme of talks and workshops is a collaboration between the University of Birmingham, UCD Child and Adolescent Psychiatry, the Diseases of Modern Life and Constructing Scientific Communities Projects at St Anne’s College, Oxford. Together we seek to explore productive interactions between narrative and mental health both historically and in the present day. Bringing together a range of interdisciplinary professionals, including general practitioners, hospital clinicians, psychiatrists, philosophers, service users, and historians of literature and medicine, we will investigate the patient experience through the prism of literature and personal narrative to inform patient-centred care and practice, and focus on ways in which literature might be beneficial in cases of burnout and sympathy fatigue.
The full programme is available here.
Registration is now open and places can be booked here.
Further information is also available here.
If you have any questions about the event, please get in touch with Dr Melissa Dickson at m.dickson@bham.ac.uk or Dr Elizabeth Barrett at elizabeth.barrett@ucd.ie.
Aristotle held that the heart was the seat of intelligence until Herophilos, one of the founders of Anatomy, showed it to be the brain. While many may see Anatomy as being a largely discovered field there is still much we can learn from the human form.
The research focus in Human Anatomy at UCD currently involves:
The one year (or possible extension for the duration of research degree) full-time scholarship programme offers an €18,000 tax-free stipend along with payment of 100% of student EU fees. Scholarships are reviewed on an annual basis and may be extended based on satisfactory progression in teaching and research. Successful candidates will undertake a graduate research degree while gaining skills and experience teaching functional and clinical anatomy to medical and allied health students. Strong academic skills and competency in Anatomy are desirable as part of the selection criteria, along with proficient communication skills. Prior clinical training is desirable but not a mandatory requirement.
Monday 5th June 2018 (5pm)
More information on this course here
Researcher: Dr. Jennifer Yates
Title of research: Understanding medical educators approach to curiosity in medical education; a qualitative interpretive study
Ethics: Ethical Approval supplied by College of Medicine, Nursing and Health Sciences Research and ethics committee, National University of Ireland, Galway [CMNHS REC, NUIG]
‘What is this research about?’
Curiosity is an enrapturing and maddening concept, it is the eternal itch that needs to be scratched. There is and has been general concern amongst medical educators that the curiosity of medical students and modern medical professionals is diminishing.
This research is about the concept of curiosity and how curiosity is approached during teaching encounters within medical education.
I aim to discuss with current medical educators what the term ‘curiosity’ means to them and how they cultivate it in their daily teaching of undergraduate medical students.
‘Who can participate?’
You are being invited to take part if you are part of the teaching staff of the school of medicine,UCD.
I am hoping to recruit educators from a range of disciplines/specialities and those with both little and lots of teaching experience.
‘What will I have to do?’
I will conduct one to one semi structured interviews lasting approximately 30-45minutes on one occasion at a time and place convenient to you.
‘When is recruitment open?’
I aim to begin interviewing participants from the end of May 2018 until early July.
Interested to know more?
If you want to know more, please contact Dr Jennifer Yates at Jennifer.yates@ucd.ie
The UCD School of Medicine is pleased to report the outcome of the 2017/2018 UCD Medicine Clinical Pathway adjunct appointment process. A total of 74 applications were received under the School’s adjunct academic appointment process comprising 44 first time applicants and 30 applications for re-appointment or promotion. Following these appointments, the School’s adjunct clinical faculty now extends to 605 hospital consultants, general medical practitioners, radiographers and paramedics from across 32 clinical sites, a nationwide general practice network, community mental health services as well as the National Ambulance Service and Dublin Fire Brigade.
As a School, we are highly dependent on clinicians within our affiliated teaching hospitals, acute, general and specialist hospitals and within primary care centres to support the delivery of the clinical training component of our education programmes and to help drive our biomedical and clinical research programmes. Clinician engagement in University business is greatly facilitated by having a formal adjunct appointment. Hence in 2008, the School introduced the UCD Medicine Clinical Pathway scheme to provide formal university acknowledgement of these contributions to academic activities, recognising that many clinicians contribute strongly despite having no protected academic time.
The School is delighted to announce that the following individuals have been appointed to the rank of UCD Full Clinical Professor:
Among those appointed to, or confirmed at the rank of UCD Clinical Professor were:
Among the 44 first time appointees in the 2017/2018 scheme, 20 were appointed at UCD Assistant Clinical Professor/UCD Clinical Lecturer and 24 were appointed at UCD Associate Clinical Professor. Of those applying for advancement to higher academic rank under the UCD Medicine Clinical Pathway, 24 of 28 promotion applications (86%) were successful with four applications recommended for continued appointment at the same academic rank. 14 UCD Assistant Clinical Professors were advanced to UCD Associate Clinical Professor rank and one UCD Assistant Clinical Professor was recommended for appointment as UCD Clinical Professor (i.e. advancement by two ranks). Six UCD Associate Clinical Professors were advanced to UCD Clinical Professor rank and one UCD Associate Clinical Professor was recommended for appointment at UCD Full Clinical Professor (i.e. advancement by two ranks) ; Two UCD Clinical Professors were recommended for appointment at UCD Full Clinical Professor (i.e. advancement by one rank) and two were recommended for continued appointment at the existing academic rank. A single applicant was recommended for appointment via the UCD Visiting Academic scheme on the basis that this individual now holds a substantive academic appointment at another Irish University.
The UCD Medicine Clinical Pathway deliberations were conducted by an academic Review Panel comprising members of the School, other UCD Schools and other Irish Medical Schools. The formal School report on the review was accepted by the College of Health & Agricultural Sciences and details of appointments and promotions will be forwarded to UCD Human Resources to update the official University records.
As part of our commitment to gender equality, we note that, consistent with previous years, approximately 30% of applicants were female. An analysis of promotion outcomes by gender after the conclusion of the review process does not indicate any differences in promotion outcome by gender. It is noted that the number of applications for promotion by males was 2.5 times greater than that from females. This ratio is consistent with the total eligible adjunct population which currently stands at 29% female and 71% male.
More Information
A full list of the appointments and re-appointments made under the UCD Medicine Clinical Pathway 2017/2018 scheme can be found here. List of Appointments under the UCD Medicine Clinical Pathway 2017/2018 scheme
A full list of all current UCD Medicine Clinical Pathway appointees can be found here. Register of UCD Medicine Clinical Pathway Appointments

Monday 14th May marked the first Skin Cancer Awareness Event at UCD. The event took place in the UCD Student Centre and was organized by SBI in collaboration with the Irish Skin Foundation, colleagues from UCD Conway Institute and BREAST-PREDICT.
Volunteers were based at a stand in the UCD Sports Centre and across the UCD Belfield Campus for this educational awareness event, which was targeted at students, staff and anyone passing by with advice on protecting their skin in the sun as well as showcasing the work undertaken by researchers in UCD. It’s one of many events as part of an international campaign, ‘Melanoma Awareness Month’ which takes place every May. The day was an immense success, with many people leaving with the central message of the importance of protecting their skin as well as information on skin cancer prevention. More than 650 leaflets on skin cancer prevention and sun cream samples were distributed on campus.
In addition, students got involved in a competition to ‘Dress up for the beach’, with prizes kindly donated by BigStyle & Sunglasses.ie.
Systems Biology Ireland has a dedicated team of researchers whose work focuses on the mechanisms that cause melanoma, to get an understanding of the resistance mechanisms involved in melanoma therapy and try to design novel therapies to combat this disease. The Irish Skin Foundation is a registered charity who supports people with skin diseases including melanoma.
In addition to this Skin Cancer Awareness Event at UCD, SBI is also raising awareness for melanoma by highlighting the work that researchers in SBI and the UCD Conway Institute do by way of a social media campaign. Please follow #UCDMelanomaAwareness for the daily updates on Twitter.
For more information:
Although it has been a worrying couple of weeks for Irish women, Professor Donal Brennan explains why it is vital for women to continue with the cervical screening programme. This article first appeared on The Journal.ie and has been reproduced with the kind permission of both the Author and The Journal.ie.
The last two weeks have been an extremely worrying time for many Irish women as awareness of, and concerns about, cervical cancer are understandable. The many sad cases of women involved in the cervical cancer audit has shaken everybody, including those involved in caring for women with cervical cancer.
Although there are many issues that remain to be answered in forthcoming reviews and investigations, it is important to separate the critical issues that have arisen as a result of the cancer review from the day-to-day workings of the screening programme.
Irish women deserve enormous credit for being so proactive about managing their health with 80% attending for smear tests under the CervicalCheck programme over the last 10 years. As a result of such high levels of attendance we have seen a progressive decrease in the incidence of cervical cancer over the last decade.
We have also seen a significant increase in the proportion of women diagnosed with early stage cervical cancer which is often cured by a small operation performed under local anesthetic – known as a LLETZ procedure. As a result of the controversy generated by the CervicalCheck cancer review, and in particular the failure to inform patients of their audit outcomes, it is clear that many people misunderstood the impact of screening, the strengths and weaknesses of the Pap smear test and how we diagnose and treat cervical cancer.
It has been known for some time that cervical cancer is caused by persistent human papilloma virus (HPV) infection. Worldwide, 80% of the population will contact HPV at some point in their lives once they become sexually active, however the vast majority of us clear the virus via our immune system.
In approximately 10% of women of reproductive age the virus persists in the cervix and causes changes in cells on cervical “skin”, which results in an abnormal smear test. Ways of reducing the risk of HPV infection include using condoms and not smoking – which reduces the immune system’s ability to clear the virus.
Persistent HPV infection causes pre-cancerous changes in the cervix, also known as cervical intra-epithelial neoplasia (CIN), which is graded from 1 (least severe) to 3 (most severe). If left untreated the risk of progression of CIN 3 to cancer is 20-30% over 10 years.
Because we understand the cause and time course of precancerous changes in the cervix the aim of screening is to detect, diagnose and remove the precancerous (CIN 3) cells before they progress to invasive cancer. We are now more confident that CIN 1 and 2 will often spontaneously regress and can be closely monitored without need to remove the precancerous cells.
Cervical cancer screening involves regular cervical smears which identify women who don’t have symptoms but who are at risk of having the aforementioned CIN. Women who have symptoms, particularly bleeding between their period or after intercourse should attend their doctor for assessment, even if they have had a recent normal smear.
A smear test involves removal of some cells from the external surface of the cervix which are placed in some liquid and transferred to a laboratory where they are examined under a microscope. Changes in the cells associated with HPV infection can be quite subtle and difficult to interpret, which means a number of different doctors or scientists could read the same smear and provide a different result.
This is why there has been such discussion in recent weeks around false negative rates and variation between different labs. This might alarm some women, however the issue is generally overcome by the fact that the rate of progression of disease from precancerous changes to cancer is slow and that is why we offer women regular smears at defined intervals (every 3 years between the age of 25 and 45).
Therefore although the smear test has significant weakness, up until recently it was the best test we had to screen large populations. It really only works in a large, well-organised, quality assured programme with call and recall systems and easy access to colposcopy clinics.
Once a smear is reported as being high grade this must be confirmed via a biopsy which is taken by a nurse or doctor in a colposcopy clinic. A smear and a biopsy are completely different tests and not every woman who has an abnormal smear will have CIN. It is also important to remember that cancer can only be diagnosed based on a biopsy, not a smear test, as smear tests are specifically designed to identify pre-cancerous cells, and a smear taken from a cancer could easily be reported as negative.
Multiple studies have demonstrated that screening for cervical cancer reduces the incidence and mortality of cervical cancer. However, even in the most established programmes in the UK and Australia which have now been in existence for over 30 years, the maximum reduction in incidence appears to be 75%.
Therefore screening is not 100% effective and unfortunately and sometimes tragically 20-30% of women who develop cervical cancer will have attended for smears all of which will have been normal.
The most common reasons for this are either the unfortunate human error associated with smear tests as outlined above but also the fact that 10-20% of cancers of the cervix are adenocarcinomas which arise from inside the cervical canal and are rarely picked up with smears which take cells from the external surface of the cervix.
Smears generally detect pre-cancerous changes associated with the much more common squamous cell carcinoma. Both adeno and squamous carcinoma are caused by HPV infection, however screening has only ever demonstrated a reduction in the incidence squamous cell carcinoma.
The last 10 years have seen two significant developments. First has been the introduction of HPV vaccination. HPV vaccination is now showing massive reductions in HPV infection rates in Scotland and Australia with associated reductions in the development of CIN as women who received the vaccine in school are now reaching their late 20s and early 30s.
We have yet to see a reduction in cervical cancer rates, but this is likely to happen over the next 5-10 years. A number of countries have introduced male vaccination which in addition to reducing the risk of penile, anal and head and neck cancers, which are all HPV related, also increases herd immunity and will have additional health benefits.
Extensive assessments of the HPV vaccine have confirmed its safety profile and a recent Cochrane review of the earliest vaccine trials, with the longest follow-up data, demonstrated that vaccine does not increase the risk of serious side effects which was about 7% in both HPV vaccinated or control (placebo) groups.
HPV vaccination will reduce the number of people in a population with HPV infection and will allow us to replace standard smears with HPV testing. Although the test will still be taken like a smear, it will be analysed in an automated fashion, giving a simple positive or negative result and will remove the risk of human error associated with standard smear tests.
It is estimated that HPV testing will reduce the false negative rate of testing to 10-15% and increase the detection of cervical cancers by 30%, which may be related to increased detection of the aforementioned adenocarcinomas. A number of countries have commenced HPV based screening including Australia, the Netherlands and parts of the UK. It is planned to proceed to HPV-based screening in Ireland in the near future.
The objective evidence we have at the moment suggests the national cervical screening programme is reducing the incidence of cervical cancer. At present the best way to reduce the risk of cervical cancer is to stay within the national programme and vaccinate your daughters.
Professor Donal Brennan is UCD Professor of Gynaecological Oncology based at the National Maternity Hospital, Mater Misericordiae University Hospital, St Vincent’s University Hospital and the UCD School of Medicine, University College Dublin. He is a consultant in obstetrics and gynaecology and a member of the Institute of Obstetricians and Gynaecologists.
This article first appeared in The Journal.ie on Monday 14th May 2018 and has been reproduced here with the kind permission of both the author and the original publisher.
A large crowd of new graduates from the UCD Medicine Classes of 2018 and their supporters gathered with staff and our clinical colleagues at UCD O’Reilly Hall on the evening of Thursday 7th June 2018 for the 2018 UCD Medicine Conferring Dinner. This black-tie event is designed to celebrate student achievement in each of our four undergraduate degree programmes (Medicine, Graduate Entry Medicine, Radiography and Biomedical, Health & Life Sciences) and the completion of their studies. Student medals and staff awards were presented by the Dean of Medicine & Head of School, Prof Patrick Murray who hosted the evening, the final UCD Medicine Conferring Dinner of his 5-year term.
In attendance were College Principal, Professor Cecily Kelleher, former Deans of Medicine, Professor Ronnie O’Regan and Professor Muiris X FitzGerald as well as UCD Medicine alumnus and former UCD Registrar, Professor Philip Nolan, currently President at Maynooth University. Prof Nolan’s daughter Rachel was among the graduating Medicine Class of 2018. In addition to representatives of our clinical training partners and our extended academic clinical faculty, we were delighted to welcome Guest of Honour, Dr Rhona Mahony.
The Dean of Medicine, Prof Murray presented the School’s Honorary Fellowship award to Dr Rhona Mahony (UCD Medicine 1994), Master at the National Maternity Hospital. The UCD Medicine Honorary Fellowship is the highest award that the School can bestow and was given to Dr Mahony in recognition of our outstanding leadership of the National Maternity Hospital over the past seven years. In accepting the award, Dr Mahony paid tribute to her many mentors throughout her own career and congratulated the graduating class as she welcomed them to the Medical profession. Dr Mahony has become something of a leadership role model for many young medical students with her warm patient-focus and courageous pursuit of excellence in healthcare.
Student of the Year Awards were presented by Professor Bill Watson (BHLS), Associate Professor Stuart Bund (Physiology), Associate Professor Jonathan McNulty (Radiography) and by Prof Fionnuala McAuliffe (Medicine), President of the UCD Medical Graduates Association.
| Programme | Student of the Year |
|---|---|
| Medicine | Dr Patrick Short |
| Radiography | Teresa Kilcoyne |
| Physiology | Amy Hassett |
| Biomedical, Health & Life Sciences | Jeremiah Nolan & Roslyn Colgan (ex-aequo) |
College Principal, Professor Cecily Kelleher presented a number of prizes from the Medicine programme including:
| Medal or Prize | Recipient |
|---|---|
| 1941 Medal | Dr Dora Gorman |
| Aongus J Curran Medal in Otolaryngology | Dr Kyle Smothers |
| Brian McGovern Perpetual Medal | Dr Niamh Conlon |
| Colman Saunders Medal | Dr Laura Mannion |
| D.K. O'Donovan Medal in Medicine | Dr Andrew Griffin |
| Geoffrey J. Bourke Medal | Dr Michael Gilligan |
| John McGrath Memorial Medal in Forensic & Legal Medicine | Dr Maura Hannon |
| Kieran O'Driscoll Prize | Dr Calvin Flynn |
| Kirwan Medal | Dr Aoife Smyth |
| Paediatrics Medal | Dr Dora Gorman |
| Prof Niall O'Higgins Medal for Surgery | Dr Calvin Flynn |
| Sean Malone Medal in Psychiatry | Dr Sarah Devlin |
| Surgeon Boyle Kennedy Medal | Dr Calvin Flynn |
| Eimear Walsh Memorial Medal | Dr Jennifer Britton |
| Lorcan Miller Memorial Medal | Dr Jennifer Britton |
The Eimear Walsh and Lorcán Miller Memorial Medals were presented at the UCD Medicine Conferring to Dr Jennifer Britton by members of the Walsh and Miller families.
Professor Kelleher also presented several medals to graduates of the undergraduate Radiography degree programme including:
| Medal | Recipient |
|---|---|
| Kate Matthews Medal | Ciara Crofton & Nicola Cleary (ex-aequo) |
| O'Farrell Medal | Maria Malone |
| Philips Medal | Andrea Burke |
| Deirdre Conroy Medal | Killian Lavelle & Ciara Skelton (ex-aequo) |
Prof Kelleher also presented a number of staff awards to members of our teaching faculty and academic support staff including:
| Award | Recipient |
|---|---|
| Medicine (Pre-Clinical) Teacher of the Year | Dr Koon-Meng Chan & Dr Peter Holloway |
| Medicine (Clinical) Teacher of the Year | Dr Paul Rush & Prof Gerard McEntee |
| BHLS Teacher of the Year | Dr Antoinette Perry |
| Radiography Teacher of the Year | Ms Marion Maher |
| Physiology Teacher of the Year | Dr Eoin Cummins |
| Technical Staff Award | Dr David Crampton |
| Administrative Staff Award | Mr Steven Masterton |
We offer our congratulations to our honorary fellow, Dr Rhona Mahony, to the graduating classes of 2018 and to the various recipients of student and staff awards. Our sincere thanks to the Health Sciences Programme Office on their organisation of the event and to all who participated.
A selection of photographs from the event are available on the School’s Flickr account (here). High resolution copies can be downloaded for personal, non-commercial use.
The 2018 UCD Medicine Conferring took place at UCD O’Reilly Hall, Belfield on Thursday 7th June 2018 with 229 graduands conferred with undergraduate entry or graduate entry Medicine (MB BCh BAO) degrees as well as 5 undergraduate Bachelor of Science and 70 graduate masters or doctoral degrees.
The proceedings were led by UCD President, Prof Andrew J Deeks and Prof Patrick Murray (Dean of Medicine and Head, UCD School of Medicine) supported by Prof Cecily Kelleher (College Principal, UCD College of Health & Agricultural Sciences).
The School was honoured to have in attendance the families of the late Dr Lorcán Miller and Dr Eimear Walsh, two students of the Class of 2018 who were among the six students killed in the 2015 Berkeley accident. Both students were conferred with posthumous awards of Honours Degree of Bachelor of Medicine, Bachelor of Surgery, Bachelor of Obstetrics (MB BCh BAO) by President Deeks.
There was a large number of academic and clinical faculty present on the dais including several who witnessed their sons or daughters received their medicine degrees. While it is not unusual for staff or alumni to have their children among the graduating class, some graduates are the first in their families to have completed third level education. Several staff members had a number of doctoral students conferred with Doctor of Medicine (MD) or Doctor of Philosophy (PhD) degrees including Prof Sabine Koelle (with 4 PhD students) and Prof Fionnuala McAuliffe (with 2 PhD students).
Several sportspersons featured among the graduating class including soccer internationalist Dr Dora Gorman (Medicine), Dublin GAA stars Dr Jack McCaffrey (Medicine) and Dr Oisín Gough (PhD) and Kilkenny GAA wing-back Cillian Buckley (MSc by Research). The group also included two UCD Ad Astra Performing Arts Scholars in Dr Oisín Friel (Music) and Dr Eithne Nic An Ríogh (Music). In addition to being conferred with her Medicine degree award, Dr Dora Gorman was conferred with a Master of Science award having completed an intercalated master’s programme. Dora also claimed the 1941 Medal (for highest GPA in the final two years of the Medicine programme) and the Paediatrics Medal (highest score in the subject of paediatrics). Eithne has also secured an Academic Internship (under the supervision of Prof Walter Cullen and Prof Jack Lambert) as have Dr Rory Plant (under the supervision of Associate Professor Suzanne Donnelly) and Dr Frank Fogarty (under the supervision of Prof Walter Cullen and Dr Geoff McCombe).
The graduates from our Medicine programmes now formally join the ranks of the medical profession whereupon they begin a year’s further supervised training as interns to complete their medical practitioner registration requirements. Many of our graduates will undertake their internship within the UCD Intern Training Network.
Graduates conferred during the 2018 UCD Medicine Conferring included:
| Degree | Number Awarded |
|---|---|
| Medicine (MB BCh BAO) | 229 |
| Bachelor of Science (BSc) | 5 |
| Master of Science (MSc) | 29 |
| Doctor of Medicine (MD) | 11 |
| Doctor of Philosophy (PhD) | 30 |
| Total Awarded | 304 |
| Student |
Thesis Title |
Supervisor |
| Kelly, Ciara |
Factors Influencing Accrual to Cancer Clinical Trials in Ireland |
Dr Catherine Kelly |
| Tuohy, Stephen |
The Clinical and Molecular Investigation of Genetic Conditions Contributing to Sudden Arrhythmic Death Syndrome in an Irish Population |
Dr Sean Ennis |
| Jordan, Emmet |
Assessment of genomic alterations in urachal and primary bladder adenocarcinoma |
Dr David Gallagher |
| Mc Mahon, Colin |
Echocardiographic Assessment of Paediatric Cardiomyopathy |
Prof Billy Bourke |
| Doyle, Fergus |
Characterisation of Anti-C6orf129, a Novel Glaucoma-associated Antibody |
Prof Colm O’Brien |
| Mavinkurve, Meenal |
Natural Killer Cell Dysfunction in Childhood and Adolescent Obesity |
Prof Donal O’Shea |
| Smith, Michelle |
The Application of Three-Dimensional Printing of Anatomy to Medical Education, Simulation Training and Clinical Practice |
Prof James Jones |
| Mc Donald, Ian |
Identification and Characterisation of Key Mediators and Receptors in Chronic Pruritus and to Compare these key Mediators in Different Pruritic Dermatoses |
Prof Martin Steinhoff |
| Farren, Maria |
A Study of the Effect of Inositol on Women at risk of Developing Gestational Diabetes Mellitus |
Prof Michael Turner |
| Keaney, John |
Neutrophil gelatinase-associated lipocalin in contrast - induced acute kidney injury - The role of novel biomarkers of renal injury in patients undergoing coronary angiography |
Prof Patrick Murray |
| Hayden, Derek |
Atrial Fibrillation Related Stroke and Transient Ischaemic Attack- Epidemiology, Secondary Prevention and Imaging Characteristics |
Prof Peter Kelly |
| Doody, Alison |
Plasma sTNFR1 and Markers of Adipose Stress and Systematic Inflammation in Patients with Diabetic Kidney Disease |
Prof Carel Le Roux |
| Crowley, Claire |
3D printing technologies and augmented reality in novel endovascular training model |
Prof James Jones |
| Mc Evoy, Catriona |
The Molecular Pathogenesis of Tubulointerstitial Fibrosis and Progressive Chronic Kidney Disease |
Dr Denise Sadlier |
| Gough, Shane |
The potential role of FRMD3 in Diabetic Kidney Disease |
Prof Catherine Godson |
| Woods, Conor |
Tissue specific glucocorticoid metabolism in obesity and the effect of glucocorticoids on invariant natural killer T cells |
Prof Donal O’Shea |
| Geraghty, Aisling |
The ROLO Kids from Pregnancy to Five Years: Insights into Maternal Nutrition, Epigenetics and Lifestyle Factors |
Prof Fionnuala Mc Auliffe |
| O'Brien, Eileen |
The ROLO Mothers from Pregnancy to Five Years: A Exploration of Maternal Dietary, Socioeconomic and Environmental Factor s |
Prof Fionnuala Mc Auliffe |
| Ortiz Meriona, Raul Antonio |
Genomics of polyploid yeasts: evolutionary insights and biotech potential |
Prof Kenneth Wolfe |
| Synott, Naoise |
Mutant p53 as a Therapeutic Target for Triple Negative Breast Cancer |
Prof Michael Duffy |
| Daly, Niamh |
A study of glucose stabilisation and the effect of an ante-natal exercise intervention on maternal glycaemia |
Prof Michael Turner |
| Dulohery, Kate |
How Excess Testosterone Impacts the Microarchitecture and Fu nction of the Oviduct - New Insights Using Cutting Edge Technologies in the Human and in a Bovine Model. |
Prof Sabine Koelle |
| Leavy, Myles |
Effects of Elevated B-estradiol Levels on the Male Reproductive Tract, Spermatoza and Sperm Oviduct Interactions in the Human and a Bovine Model |
Prof Sabine Koelle |
| Eseoghene, Itagar (Loveth) |
Inflammation of the Bovine Fallopian Tube: Effects on Tubal Functional Morphology and Gameto-Maternal Interaction |
Prof Sabine Koelle |
| Hughes, Barbara |
Mechanisms of Human Sperm Oviduct Interaction |
Prof Sabine Koelle |
| Olszewska, Diana Angelika |
Genetics and Biomarkers in Parkinson's Disease in Ireland |
Prof Timothy Lynch |
The proceedings concluded with the awarding of the inaugural Lorcán Miller medal and Eimear Walsh medal to Dr Jennifer Britton by members of Lorcán and Eimear’s families.
A selection of photographs from this event is available on the School's Flickr account for private, non-commercial use.
Is birth weight the major confounding factor in the study of gestational weight gain?: an observational cohort study
There has been much interest on both maternal obesity and gestational weight gain (GWG), particularly on their role in influencing birth weight (BW). Several large reviews have reported that excessive GWG’s associated with an increase in BW. However recent large, well-designed, randomized controlled trials studying interventions aimed at reducing GWG have all consistently failed to show a reduction in BW despite achieving a reduction in GWG.
Researchers at the UCD Centre for Human Reproduction at the Coombe Women and Infants University Hospital have published the results of an observational cohort study of the topic. The aim of the longitudinal prospective study was to examine the relationship between GWG and birth weight in women where GWG and Body Mass Index (BMI) were measured accurately in a strictly standardised way.
A total of 522 women were enrolled at their convenience before 18 week gestation with height and weight accurately measured at the first antenatal visit. Maternal weight was measured again after 37 weeks gestation and the weight of the baby was measured at birth. Body Mass Index was calculated and the relationship between GWG and BW was analysed.
The group concluded that the positive correlation between GWG in pregnancy and BW can be accounted for by the contribution of fetal weight to GWG antenatally without a contribution from increased maternal adiposity. There was a wide range of BW irrespective of the degree of GWG and obese women had a lower GWG than non-obese women. These findings help explain why Randomized Controlled Trials (RCTs) designed to reduce GWG have failed to decrease BW and suggest there is no causative link between excessive GWG and increased BW.
Is birth weight the major confounding factor in the study of gestational weight gain?: an observational cohort study
Amy C. O’Higgins, Anne Doolan, Thomas McCartan, Laura Mullaney, Clare O’Connor and Michael J. Turner BMC Pregnancy and Childbirth (2018) 18:218 https://doi.org/10.1186/s12884-018-1843-9 [link]
Throughout our School’s history, we’ve a proud tradition of students, staff and alumni representing their clubs, county and university in Gaelic Games. So in the run up to Gaelic Sunday and the business end of this year’s All-Ireland Football Championships, we thought we’d try to put together a UCD Medicine dream team.
We invite you to nominate players – male or female - of any county in any era, who were students, staff or graduates of the School and who represented their county at underage, minor or senior level football for inclusion in our 30-person squad.
Please also suggest an ideal squad position for your nominee. Note: we do not anticipate deploying a sweeper in our team!
We’ll warn you that we’ve already identified a strong squad of players, supported by an equally impressive and experienced back room team. However the latter want to leave no stone unturned in the search of the dream team that makes up the UCD Medicine Harps.
Our team boast an impressive total of All Ireland medals and contains players who made real impact on the sport. We’ve had flying doctors and surgeons who have been known to fly off the handle. We’ve had Players of the Year and Players on the Team of the Millennium. Sure isn’t the premier higher education intervarsity competition named after one of our own (Sigerson Cup) and another of our graduates even introduce the solo to gaelic games!
Put your thinking caps on and let us know who we should consider for selection. If you have some pen profiles on the players, we’d gratefully welcome these also to help with our selection.
Entries must be received by Friday 10th August 2018. Thereafter the Committee will consider the nominees and will name its first squad in the lead up to the All-Ireland Football Final.
Nominees to comms.medicine@ucd.ie ; #GRMA. #FunFriday #UCDMedHarps
Multi-centre clinical research collaborations are essential to advancing our understanding of complex haematological conditions, particularly those which are relatively rare in nature. One such condition is dyskeratosis congenita, a genetic multisystem disorder with frequent involvement of the bone marrow. Dyskeratosis congenita can also present concomitantly with pulmonary fibrosis, liver abnormalities, neurological, gastrointestinal, ocular impairment and cancer predisposition. The causative mechanism of the disease is abnormal telomere shortening due to a defect in one of the genes encoding for the telomerase-shelterin complex. Haematopoietic stem cell transplantation (HSCT) is the only definitive cure to restore haematopoiesis in dyskeratosis congenita, even though it cannot correct other organ dysfunctions.
A team of international investigators supported by researchers from Our Lady’s Children’s Hospital Crumlin, examined the outcome of HSCT in the largest cohort of DC (n = 94) patients ever studied and who had received allogeneic HSCT between 1979 and 2015. The retrospective, multi-centre study showed that overall survival (OS) and event-free survival (EFS) at 3 years after HSCT were 66% and 62%, respectively. Multivariate analysis showed better outcomes in patients aged less than 20 years and in patients transplanted from a matched, rather than a mismatched, donor. OS and EFS curves tended to decline over time.
Early lethal events were infections, whereas organ damage and secondary malignancies appeared afterwards, even a decade after HSCT. A non-myeloablative conditioning regimen appeared to be most advisable. Organ impairment present before HSCT seemed to favour the development of chronic graft-versus-host disease and T-B immune deficiency appeared to enhance pulmonary fibrosis. According to the present data, HSCT in DC is indicated in cases of progressive marrow failure, whereas in patients with pre-existing organ (particularly lung) damage, this should be carefully evaluated as it may increase the risk of graft-versus-host disease and worsen survival.
The investigators conclude that HSCT might be an option in subjects affected by dyskeratosis congenita and bone marrow failure, but it is associated with a high risk of early and late mortality due to infections, organ damage and secondary malignancies. They believe that the indication for HSCT in dyskeratosis congenita patients with bone marrow failure need to be established on an individual basis after thorough evaluation of lung and non-haematological organ damage.
Original Article
Outcome of haematopoietic stem cell transplantation in dyskeratosis congenita.
Fioredda F, Iacobelli S, Korthof ET, Knol C, van Biezen A, Bresters D, Veys P, Yoshimi A, Fagioli F, Mats B, Zecca M, Faraci M, Miano M, Arcuri L, Maschan M, O'Brien T, Diaz MA, Sevilla J, Smith O, Peffault de Latour R, de la Fuente J, Or R, Van Lint MT, Tolar J, Aljurf M, Fisher A, Skorobogatova EV, Diaz de Heredia C, Risitano A, Dalle JH, Sedláček P, Ghavamzadeh A, Dufour C.
Br J Haematol. 2018 Jul 9. doi: 10.1111/bjh.15495. PMID: 29984823
A team of international researchers, including Professor Owen Smith (UCD Professor of Paediatric and Adolescent Haematology) have demonstrated that genome instability in bone marrow failure patients with biallelic ERCC6L2 variants arises due to a particular genetic mutation causing a primary transcription deficiency rather than as a consequence of a DNA repair defect.
Bone marrow failure is an inherited life-threatening condition characterised by defective blood cell formation, developmental abnormalities and predisposition to cancer. Individuals affected by inherited bone marrow failure syndromes present with a variety of hematological complications. These complications include myelodysplastic syndrome and acute myeloid leukemia.
Bone marrow failure caused by biallelic variants in the ERCC excision repair 6 like 2 gene (ERCC6L2) is considered to be a genome instability syndrome with DNA repair compromised in cells. The data from this study indicates a mechanism in bone marrow failure in which patients with ERCC6L2 mutations are defective in the repair of transcription-associated DNA damage.
Researchers have shown that patient-derived lymphoblastoid cell lines exhibit hypersensitivity to DNA damaging agents that specifically activate the transcription coupled nucleotide excision repair (TCNER) pathway. These patients’ cell lines are also hypersensitive to transcription inhibitors that interfere with RNA polymerase II. These patient cell lines are compromised in DNA repair capacity, display abnormal delay in RNA synthesis recovery rates, and fail to accurately stall transcription elongation following treatment with a transcription inhibitor.
The researchers have demonstrated that ERCC6L2 contributes to the DNA damage response through its interaction with an enzyme called DNA-dependent protein kinase (DNA-PK) and that it occupies gene bodies alongside RNA polymerase II. They also observed an increase in nucleoplasmic R-loop density, which could be the cause of the genomic instability.
DNA-PK was initially identified as a regulatory component of transcriptionally poised RNA polymerase II. As transcription is a fundamental mechanism behind cell fate, the role of DNA-PK in regulating this process may have critical implications in bone marrow failure.
This research suggests that the interaction between ERCC6L2 and DNA-PK could be particularly relevant in the repair of transcription-associated DNA lesions. These findings support the notion of a primary transcription defect rather than a DNA repair defect in patients with BMF caused by the ERCC6L2 genetic mutation.
Tummala H, Dokal AD, Walne A, Ellison A, Cardoso S, Amirthasigamanipillai S, Kirwan M, Browne I, Sidhu JK, Rajeeve V, Rio-Machin A, Seraihi AA, Duncombe AS, Jenner M, Smith OP, Enright H, Norton A, Aksu T, Özbek NY, Pontikos N, Cutillas P, Dokal I, Vulliamy T.
Proc Natl Acad Sci U S A. 2018 Jul 9. pii: 201803275. doi: 10.1073/pnas.1803275115. PMID:29987015
Researchers from the UCD Centre for Human Reproduction report a study comparing the maternal dietary intake of smokers with non-smokers at the mothers’ first perinatal visit. They demonstrated serious dietary inadequacies among smoking mothers which may aggravate fetal growth restriction and highlight the importance of promoting smoking cessation interventions in pregnancy and the need for dietary interventions in women who continue to smoke.
The cross-sectional study was conducted alongside researchers from the DIT School of Biological Sciences and the Trinity College School of Medicine between June 2014 and March 2016 and was published in the British Medical Journal.
Researchers compiled the dietary intakes of both macro and micronutrients for 398 women at their first prenatal visit, recruited opportunistically after sonographic confirmation of an ongoing singleton pregnancy. At this time the women also self-reported whether they were non-smokers or continued to smoke during pregnancy.
Maternal smoking is strongly associated with an increase in adverse pregnancy outcomes, including increased risk of intrauterine growth restriction. This risk increases in accordance with the number of cigarettes smoked, and cessation of smoking in the first half of pregnancy may normalise fetal growth. Fetal growth is also influenced by deficiencies in maternal macro and micronutrients.
A correlation was found between maternal smoking status and diet. Specifically, women who continued smoking during pregnancy were found to have serious inadequacies of both dietary micronutrients and macronutrients. These inadequacies could potentially aggravate fetal growth restriction caused by direct toxicity from cigarettes. Women who had stopped smoking had dietary intakes which compared favourably with women who never smoked. These results strengthen the case for screening for smoking in early pregnancy and offering supports for smoking cessation. These results also indicate a need to advise women who continue smoking during pregnancy about healthy eating behaviours and folic acid supplementation.
Eimer G O'Malley, Shona Cawley, Ciara M E Reynolds, Rachel A K Kennedy, Anne Molloy, Michael J Turner
O'Malley EG, et al. BMJ Open 2018;8:e021721. doi:10.1136/bmjopen-2018-021721
UCD Surgical Society invites you to submit your abstract in any surgical topic for the annual SurgSoc Conference: Stepping Up To The Table taking place on the 1st December 2018 at St Vincent's University Hospital. Submisions can include audits or research. Students from all colleges are welcome to submit an abstract.
Up to three abstracts will be selected for an oral presentation. There are also prizes that will be awarded for the categories listed in the poster above.
Abstract guidelines are as follows:
Please submit your abstracts according to the guidelines in the poster to ucdsurgicalsociety@gmail.com
For more information you can contact us via our email or our Facebook Page.
Deadline: Early November
The UCD Surgical Society's annual conference, ‘Stepping up to the Table’ is planned for December 1st 2018, with the exact date to be set in the coming weeks. This conference is a one-day student-led surgical conference, aiming to deliver interesting, educational, and engaging lectures, poster presentations, and workshops in order to promote interest in the surgical profession among medical students at UCD and other medical schools. The event will be hosted in St. Vincent’s University Hospital. We are aiming for an attendance of 125 medical students and hospital staff, which we have surpassed each time this conference has been hosted. There will be a panel of 5 speakers who are surgeons from St.Vincent’s University Hospital and Mater Misercordiae Hospital. The conference will be run on a national level and we are extending an invitation to students from all medical institutions in Ireland.
For more information about the UCD Surgical Society, check out their Facebook page.
A reminder that if you have a new student commencing in September 2018, please submit completed applications to medicine.research@ucd.ie by 30th August 2018 for September registration.
The next thesis submission date for Graduate Research Students is Friday, 7th September 2018.
Students are required to submit three soft bound copies of their thesis together with a signed thesis submission form (available here) to Student Desk in Tierney building, UCD, Belfield.
Please click here for the opening hours and map for the Student Desk.
If students are intending to submit in September 2018, supervisors are advised to forward the completed examiner nomination form for review by the relevant Boards and ACCE meetings by the following submission deadlines:
2017/18 PhD MSc External Examiner Nomination Form should be submitted to medicine.research@ucd.ie.
PhD STAGE 1 TRANSFER PROCESS - October 2018
The PhD Stage 1 to Stage 2 Transfer Process is run twice a year.
Full-time students who registered for PhD studies in September 2017 and part-time students who registered in September 2016 will be required to undertake this assessment process in October 2018
However, there are other categories of student, who may not be included on the current list of registered PhD students, who may also be required to undergo this assessment.
These may include:
For students who would be eligible for a Stage 1-Stage 2 transfer in October 2018, supervisors are advised to email medicine.research@ucd.ie by Friday 31st August 2018, so that these students can be included in Medicine Research's planning for the October assessment.
REMINDER - Doctoral Studies Panel MEETINGS
A reminder that three DSP meeting are required in the first year of students' registration.
The first meeting of a student’s DSP is organised by the principal supervisor within 3 months of the student’s initial registration, the panel should also meet at 6 months and at 12 months post registration.
Please note that it is also now mandatory that in addition to the three DSP meetings that occur in the first year of a PhD that at least one DSP meeting occurs each year thereafter.
The focus of these meetings should be on the progression of students' work and their ability to take responsibility for their own project, use initiative and critically analyse and discuss the results. Signed RPDP forms must be submitted to the school research office each year.
Please note it is the responsibility of the student and the supervisor to ensure that the DSP meetings take place.
Forms to record DSP meetings can be downloaded from here (Download College of Science & College of Health and Agricultural Sciences forms).
Please return completed DSP reports to medicine.research@ucd.ie for the student file.
2018/2019 PhD Application Form
2018/2019 MSc Application Form
The above information is presented here for information purposes and does not represent the official or complete repository of information on Graduate Research Studies at UCD. The School cannot accept any responsibilities for any change in information or closing dates which may be made by the University. For further information please contact UCD Medicine Research.
As he concludes his term as Dean of Medicine and Head of School, we take this opportunity to thank Professor Patrick Murray for his outstanding leadership and for his tremendous support to our students and staff over the past five years. It has been our distinct pleasure and honour to serve under a man of such intellect, integrity and good humour. We are delighted that Pat will resume his original duties and so we will be able to continue to benefit from his wise counsel and insight.
During his tenure as Dean of Medicine and Head of School, Pat has prioritised support to students and staff ensuring the highest quality of education and training as well as encouraging fundamental biomedical and clinical translational research. He has overseen the continued expansion of our Medicine programmes, diversifying student intake such that our students are now drawn from 40 overseas countries. He has supported the increased intake to our undergraduate Radiography programme from 40 per annum to 100 per annum to meet increased clinical workforce needs and introduced a number of new graduate taught and graduate research programmes.
In partnership with Dr Peter Doran, he has substantially expanded our educational offerings in clinical and translational research, introducing a number of highly regarded courses in partnership with industry. Notwithstanding difficult research funding environment, during his tenure, the School has maintained an average of 16M of external research funding per annum and has grants under management to the value of 81M. The School has reported its most profitable years, returning substantial financial surplus to the University despite cuts in Exchequer funding. In 2016, the School featured in the Times Higher Education World University Rankings Top 100 for Clinical, Pre-Clinical and Health Subject Area, the only Irish University to do so.
Prof Murray's term as Dean was characterised by strong support to our students who he encouraged to academic excellence and extra-curricular pursuits. He developed several new international elective opportunities and built strong connections with overseas medical schools. His willingness to engage with students on their terms was perhaps best exemplified by his participation in the Student/Staff Soccer competition and the L&H Society Debates. He led the School with great dignity and sensitivity during a number of student tragedies including the loss of life following the Berkeley Accident, the loss of a parent in the Tunisian terror attack and the death of a classmate. His support to students and staff alike during these difficult times was greatly appreciated and is a testiment to his character. His self-deprecating nature and his gentle encouragement has seen many staff assume leadership roles within the School and he has been a strong supporter of the School's Equality, Diversity and Inclusion objectives.
Building on his work as Associate Dean for International Relations, Pat continued to develop several international initiatives including the 'Introduction to the Pratice of American Medicine' in conjunction with Harvard Medical School, our clinical research masters in conjunction with Shenzhen University and oversaw the awarding of Foreign University Branch Campus status by the Malaysian Government to Penang Medical College.
Prof Murray was Chair of Irish Medical Schools Council, Penang Medical College and UCD Charles Institute. He build strong and effective collaborative links with other Irish Medical Schools and Chaired the UCD Clinical Research Centre. Despite his many administrative responsibilities, he maintained a significant teaching role and research profile.
We are pleased to report that Prof Murray is not retiring and we will continue to enjoy his company and benefit from his wise counsel as he resumes his duties as Professor of Clinical Pharmacology. We would also like to take this opportunity to thank his wife, Trish and his children for sharing their husband and father with the School.
Prof Murray is UCD Professor of Clinical Pharmacology and Consultant Physician (Clinical Pharmacology and Nephrology) at the Mater Misericordiae University Hospital, a role he took up in 2008. A graduate of the UCD Medicine 1988, Pat has had a distinguished career as a doctor, researcher, teacher and, in latter years, academic administrator.
Following his internship at the Mater Misericordiae University Hospital in Dublin, he completed a residency in internal medicine at Hennepin County Medical Center in Minneapolis, Minnesota, USA. He completed fellowship training programs in nephrology, critical care medicine, and clinical pharmacology at the University of Chicago Hospitals in Chicago, Illinois, USA.
He is board-certified in internal medicine, nephrology, critical care medicine, and clinical pharmacology. He practiced as an intensivist, nephrologist, and clinical pharmacologist at the University of Chicago Hospitals from 1996–2008, serving as the fellowship training programme director in nephrology, also directing the Acute Dialysis Service.
He has a longstanding interest in research and education to improve the prevention, diagnosis, and therapy of acute kidney injury and nephrotoxicity, and the pharmacotherapy of patients with kidney disease. He is a member of several international consensus groups that have produced guidelines for research and practice in the field of acute kidney injury (ADQI, AKIN, KDOQI).
Following his return to Ireland in 2008, Pat was appointed UCD Professor of Clinical Pharmacology and Consultant in Nephrology & Clinical Pharmacology at the Mater Misericordiae University Hospital. He has chaired of the Mater Misericordiae University Hospital Drugs & Therapeutics Committee. He is the Clinical Director of the UCD-Mater Clinical Research Centre. In 2011, he was appointed as the School's Associate Dean for International Affairs and in 2012, he was appointed Director of the Dublin Centre for Clinical Research (DCCR) Consortium Network. He was appointed Dean and Head of the School in December 2012.
Investigations by Prof Michael Keane’s group into the genetic profiles and functional characteristics of different myofibroblasts types has confirmed significant inter-population variability. The St Vincent’s University Hospital research group hope that these differences might lead to potential therapeutic targets in idiopathic pulmonary fibrosis (IPF).
Idiopathic pulmonary fibrosis (IPF) is a chronic progressive interstitial pneumonia that is characterized by excessive fibroproliferation. Myofibroblasts are key effector cells in IPF that are recruited from three potential sources: resident fibroblasts, fibrocytes and epithelial cells. The investigators hypothesized that IPF myofibroblasts from these different sources of origin might display unique genetic profiles and distinct functional characteristics.
The group activated primary human pulmonary fibroblasts (normal and IPF), fibrocytes and epithelial cells into myofibroblasts using the pro fibrotic factors TGF β and TNF α and characterised the resulting myofibroblasts using cell proliferation, soluble collagen, ELISA and contractility assays, and human fibrosis PCR arrays. They also validated genes of significance in whole human lung and by immunohistochemistry on human lung sections.
Fibroblast-derived myofibroblasts exhibited the highest expression increase in pro fibrotic genes, and genes involved in extracellular matrix remodelling and signal transduction. Functional studies demonstrated that myofibroblasts derived from fibrocytes expressed most soluble collagen and CCL18 but were least proliferative of all myofibroblast progeny. Activated IPF fibroblasts displayed highest contraction and highest levels of CCL2 production.
This study published in the American Journal of Physiology – Lung Cellular and Molecular Physiology has identified novel differences in both gene expression and functional characteristics in different myofibroblast populations. Further investigation into the myofibroblast phenotype may lead to potential therapeutic targets in the future field of IPF research.
Novel Differences in Gene Expression and Functional Capabilities of Myofibroblast Populations in Idiopathic Pulmonary Fibrosis
Sinead M Walsh, Julie C Worrell, Aurelie Fabre, Boris Hinz, Rosemary Kane, and Michael P Keane
The current approach in Ireland of screening expectant mothers for preeclampsia after they show early signs of the condition may not offer the best outcome for mothers and babies.
New UCD research published in BMJ Open (British Medical Journal) shows that women in Ireland are open to taking a low daily dose (75mg) of aspirin from early pregnancy to reduce their chances of developing the condition.
It is widely accepted that low doses of aspirin can significantly reduce the early onset of preeclampsia during pregnancy
Few studies have assessed the acceptability of non-routine medications in pregnancy. The findings of the study offer an encouraging sign that women in Ireland at low-risk of developing preeclampsia are willing to take preventive steps early in their pregnancies.
One of the study authors, Professor Fionnuala McAuliffe from the UCD School of Medicine, University College Dublin, is calling for a widespread randomised controlled trial to test the efficacy and safety of a universal low dose aspirin approach.
Preeclampsia impacts one in ten first-time pregnancies, and the warning signs can often go unnoticed causing serious problems for mother and baby.
For the mother, it can lead to acute problems of the liver, kidneys, brain and clotting system and survivors of preeclampsia have increased risk of cardiovascular and metabolic diseases later in life.
A quarter of all babies born to mothers with preeclampsia are growth restricted and a third are born prematurely.
Preeclampsia usually occurs during the second half of pregnancy, from around week 20, and the only treatment is to induce labour and deliver the baby.
“Our study investigated if women were open to taking a low daily dose (75mg) of aspirin from early pregnancy (11 weeks) and would continue to do so up until the third trimester,” says UCD Professor Fionnuala McAuliffe, a consultant obstetrician and gynaecologist at the National Maternity Hospital and Director of UCD Perinatal Research Centre.
“We found that when encouraged by their doctor to take a low-level daily dose of aspirin (75mg) from 11 weeks until 36 weeks the majority of women did so at an average adherence rate of 90%,” she explains.
The study involved 546 pregnant women from across two maternity hospitals in Dublin.
It was funded by Health Research Board, Mother and Baby Clinical Trials Network, and Perinatal Ireland.
While the women who received aspirin as part of the study reported a slight increase in vaginal bleeding, both during and following pregnancy, this did not impact on pregnancy outcome.
Internationally, there is no consensus on which screening method is best, or which women meet the criteria for aspirin use.
Another study carried out in 2017 based on pregnant women involved in the SCOPE (Screening for Pregnancy End Points) project found that complications caused by preeclampsia cost the HSE upwards of €9 million annually, with postnatal care being the largest contributor to these costs.
The Preeclampsia Foundation, a US-based NGO, reports that preeclampsia, and other hypertensive conditions, account for 76,000 maternal deaths and 500,000 infant deaths worldwide every year.
The World Health Organisation rates the condition as one of the leading causes of infant mortality and maternal death worldwide.
Reproduced with kind permission from UCD University Relations.
Congratulations to Dr Tom Wall (from Professor Donal Buggy’s group) who received the College of Anaesthetists of Ireland (CAI) Anaesthetic Research Fellowship for his presentation on The Effect of Anaesthetic Agents on Metastasis in a Mouse Model of Breast Cancer which won the research group a Scholarship prize of €25,000. Dr Wall was presented with the Fellowship by CAI President Professor Kevin Carson at the Annual CAI Congress. The award, previously named the Abbvie Scholarship in Anaesthetic Research, is funded by Abbvie and is awarded to support original research by an Irish non-consultant anaesthetist.
Applications are open from January and presentations are held in during the Annual Congress. The competition is advertised by the Education Department (CAI), application information is available on the College website. The scholarship is advertised to all trainees who are contacted directly application information is also distributed around all training hospitals.
Previous Winners of this award include:
| 2018 |
Dr Tom Wall, ‘The Effect of Anaesthetic Agents on Metastasis in a Mouse Model of Breast Cancer’. |
| 2017 |
Dr Stephen Duff, ‘Development and comparative analysis of a novel 3-D printed epidural anaesthesia simulator’. |
| 2016 |
Joint Winner: Dr David Moore, ‘An investigation of the effect of pulsed radiofrequency treatment (PRF) of the dorsal root ganglion (DRG) on cerebrospinal fluid cellular and neuropeptide concentrations and Dr Mark Johnson, ‘Can perioperative lidocaine reduce metastasis in a mouse model of breast cancer?’. |
| 2015 |
Drs Colm Keane, ‘Cell therapies for Sepsis’ and Dr Kirk Levins, Effect of anaesthetic technique on immune cell infiltration in breast cancer: A prospective, ramdomised, investigator - masked study’ |
| 2014 |
Dr Anne Doherty ‘Apelin, Placental Growth Factor and Soluble fms-like tyrosine kinase-1 at 14-16 weeks gestation in Pregnancies Complicated by early Preeclampsia and/or Fetal Growth Restriction.’ |
| 2013 |
Dr Caroline Larkin ‘The Mechanisms of sepsis-associated thrombocytopenia and thrombosis’ and Dr Noelle Murphy ‘The Validation of urinary biomarkers of acute kidkney injury (AKI) post open aortic abdominal aneurysm repair’ |
| 2012 |
Dr Noelle Murphy ‘The role of gremlin in the evolution of the acute respiratory distress syndrome’ and Dr Grace Donnelly ‘What is minimum training required for anaesthetists to be able to perform rigid bronchoscopy? A study in manikins’ |
| 2011 |
Dr Robert Grealy for his presentation entitled ‘Transcriptomic Profiling of Monocytes in Sepsis’ |
| 2010 |
Dr Stephen Frohlich “Signaling Pathways that Protect against lung damage in the acute respiratorydistress syndrome: Creb Responsive Genes in the Lung” and Dr Mairead Hayes “Determination of the potential for mesenchymal stem cells to reduce injury and enhance repair following sepsis induced Acute Lung Injury”. |
| 2009 |
Dr Ivan Hayes ‘“Intralipid in Asphyxial Cardiac Arrest- A Laboratory Study’ & Dr Criona Walsh ‘Volatile Anaesthetics nd Cardioprotectinon: The Role of Redox – Sensitive Inducible Modulators of Mitochondrial Energetics’ |
| 2008 |
Dr Tanya O’Neill ‘Post – Operative Cognitive Dysfunction: The Contribution of General Anaesthetic Agents to its Aetiology and the Role cognition enhancing drug therapies in mitigating its development’ |
| 2007 |
Dr Roger McMorrow and Dr Pádraig Mahon |
| 2006 |
Dr Martin Duffy ‘Modulation of endothelial dysfunction in the development of sepsis-induced acute long njury by hydroxyl-methyl coenzyme areductase in inhibition with simvastatin’ |
| 2004/2005 |
Dr Alistair Nichol ‘Characterization of the molecular mechanisms underlying the protective effects of Hypercapnic Acidosis in Acute Lung Injury’ |
Researchers at the Moorfields Eye Hospital NHS Foundation Trust, DeepMind Health and University College London (UCL) have developed an artificial intelligence (AI) system that can recommend the correct referral decision for over 50 eye diseases as accurately as world-leading experts, it is claimed.
The breakthrough research, published online by Nature Medicine, describes how machine learning technology has been successfully trained on thousands of historic de-personalised eye scans to identify features of eye disease and recommend how patients should be referred for care.
It is hoped that the technology could one day transform the way professionals carry out eye tests, allowing them to spot conditions earlier and prioritise patients with the most serious eye diseases before irreversible damage sets in. More than 285 million people worldwide live with some form of sight loss. Eye diseases remain one of the biggest causes of sight loss, and many can be prevented with early detection and treatment.
The research has been led by UCD Medicine alumnus, Dr Pearse Keane who is a consultant ophthalmologist at Moorfields Eye Hospital NHS Foundation Trust and NIHR Clinician Scientist at the UCL Institute of Ophthalmology.
“The number of eye scans we’re performing is growing at a pace much faster than human experts are able to interpret them. There is a risk that this may cause delays in the diagnosis and treatment of sight-threatening diseases, which can be devastating for patients.
“The AI technology we’re developing is designed to prioritise patients who need to be seen and treated urgently by a doctor or eye care professional. If we can diagnose and treat eye conditions early, it gives us the best chance of saving people’s sight. With further research it could lead to greater consistency and quality of care for patients with eye problems in the future.”
The study, which was launched in 2016, investigated whether AI technology could help improve the care of patients with sight-threatening diseases, such as age-related macular degeneration and diabetic eye disease. Using two types of neural network – mathematical systems for identifying patterns in images or data – the AI system quickly learnt to identify ten features of eye disease from highly complex optical coherence tomography (OCT) scans. The system was then able to recommend a referral decision based on the most urgent conditions detected. To establish whether the AI system was making correct referrals, clinicians also viewed the same OCT scans and made their own referral decisions. The study concluded that AI was able to make the right referral recommendation more than 94% of the time, matching the performance of expert clinicians.
The AI has been developed with two unique features which maximise its potential use in eye care. Firstly, the system can provide information that helps explain to eye care professionals how it arrives at its recommendations. This information includes visuals of the features of eye disease it has identified on the OCT scan and the level of confidence the system has in its recommendations, in the form of a percentage. This functionality is crucial in helping clinicians scrutinise the technology’s recommendations and check its accuracy before deciding the type of care and treatment a patient receives.
Secondly, the AI system can be easily applied to different types of eye scanner, not just the specific model on which it was trained. This could significantly increase the number of people who benefit from this technology and future-proof it, so it can still be used even as OCT scanners are upgraded or replaced over time.
The next step is for the research to go through clinical trials to explore how this technology might improve patient care in practice, and regulatory approval before it can be used in hospitals and other clinical settings. If clinical trials are successful in demonstrating that the technology can be used safely and effectively, Moorfields will be able to use an eventual, regulatory-approved product for free across all 30 of their UK hospitals and community clinics, for an initial period of five years.
Dr Pearse Keane graduated from UCD with an MB BCh BAO and a BMedSc in 2002 and he completed a MSc in Physiology in 2004. He was awarded an MD by the University in 2011 for his research under the supervision of Prof Colm O’Brien into the development of novel techniques in retinal imaging and their application to macular disease. He is a frequent visitor to Ireland and has acted as an external examiner in Ophthalmology for the School for several years. We congratulate Dr Keane and his colleagues on this success and wish them continued success as they seek to bring this approach into routine clinical practice.
We asked a number of our academic staff to comment on the significance of this paper. Please note none of these individuals are involved in this published research.
Prof Catherine Godson, Director of the UCD Diabetes Complications Research Centre observed,
There is a global epidemic of diabetes. It is currently estimated that there are 425 million people living with diabetes. This figure is predicted to rise to 700 million in the next decade. Diabetes is a leading cause of blindness. Earlier diagnosis will facilitate more effective and treatment and disease management. Given the prevalence of diabetes and its serious life limiting complications including kidney disease, heart disease and stroke applications of AI have huge potential benefit in earlier detection, understanding and disease management.
Prof Colm O’Brien, UCD Professor of Ophthalmology and consultant ophthalmologist at the Mater Misericordiae University Hospital commented,
These results are exciting for ‘screening’ large populations to detect sight threatening retinal diseases like diabetic retinopathy and macular degeneration – early detection and treatment where appropriate will mean that fewer patients will become visually impaired in the future – that’s the key take home message from this research paper.
The next challenge for the group will be to see if AI can help monitor patients with established disease in our clinics, and identify those at risk of progression. Also, this AI will also be very valuable at early detection of other ocular conditions such as glaucoma by examination of the optic nerve using the same OCT scans. Given the widespread use of high powered smartphone cameras, AI might well find further applications.
Mr David Keegan, UCD Clinical Professor in Ophthalmology and Retina at the Mater Misericordiae University Hospital, Mater Private Hospital and Temple Street Children’s University Hospital noted,
Pearse has become one of the world authorities on retinal imaging and his technical expertise and knowledge is well recognised. We hope to establish this type of infrastructure alongside the National Diabetic Retinal Screening Programme (RetinaScreen) in the future. The challenges are ensuring low false negatives (to ensure safety) but also to ensure low false positives to retain the integrity of the Programme and not swamp our treatment clinics with unnecessary referrals. We are making good steady progress in this regard since the Programme was established in 2013. As we have done with surveillance screening we will likely run a parallel pilot Programme using the best evidenced/positioned AI system.
De Fauw J, Ledsam JR, Romera-Paredes B, Nikolov S, Tomasev N, Blackwell S, et al. Clinically applicable deep learning for diagnosis and referral in retinal disease. Nature Medicine. 2018. [link]
RCSI & UCD Malaysia Campus (RUMC), formerly Penang Medical College (PMC) was officially launched by Minister Richard Bruton T.D., Minister for Education and Skills. The institution’s upgrade to Foreign University Branch Campus was approved by the Malaysian MOE in March this year with its full name Royal College of Surgeons in Ireland (RCSI) and University College Dublin (UCD) Malaysia Campus.
The launch at the University’s Penang campus was also attended by Deputy Director General of Higher Education, Ministry of Education Malaysia, Dr Mohd Nor Azman Bin Hassan, along with the Irish Ambassador to Malaysia, His Excellency Eamon Hickey; President of the Royal College of Surgeons in Ireland (RCSI), Mr Kenneth Mealy; Deputy President of University College Dublin (UCD), Professor Mark Rogers; and hosted by RUMC President & CEO, Professor Stephen Doughty, together with Vice President (Academic Affairs) & Registrar, Professor David Whitford and the Dean, Professor Mr Premnath Nagalingam.
Prof Stephen Doughty commented
“As we celebrate this momentous achievement as the first of many RUMC milestones we know that we are building upon more than 20 years of PMC’s high quality Irish education delivery. We continue to support the development of healthcare in Malaysia and were delighted to recently sign a MoU with the Ministry of Health to establish a new pathway for Family Medicine training for doctors in Malaysia”.
The University is committed to offer more high quality, internationally recognized programmes to cater to the growing demands in the global healthcare sector.
Established for more than 20 years ago, the institution provided Malaysia’s first registrable medical degree from a Malaysian private higher education institution and is owned by Irish institutions, the Royal College of Surgeons in Ireland (RCSI) and University College Dublin (UCD). Degrees are awarded by the National University of Ireland and are globally recognised. RUMC will continue to build on this history and will offer a high-quality Irish medical degree as well as other healthcare and related programmes at foundation, bachelors, masters and doctoral levels.
The event today was attended by many in the healthcare and education sector RUMC staff and students joined in the celebration.
The newly launched institution will be better placed to inform the profession and the public about medicine, especially through hosting the prestigious Cochrane Malaysia network which focusses on dissemination of evidence-based medicine. In addition, future plans to continue to increase research activity and output will ensure that Malaysia stays at the cutting edge of medicine development. Core activities will remain as providing high quality, affordable Irish medical education in Malaysia and ensuring that our location in the northern corridor supports the region and its development.
Nearly 1,700 medical doctors have graduated from the institution with globally recognised medical degrees of the National University of Ireland (NUI) and practice in Malaysia, Brunei, Singapore, Ireland, UK, Switzerland, Malta, Australia, New Zealand, USA and many other countries. The graduating class of 2019 will be the first to graduate under the new University name.
About RCSI & UCD Malaysia Campus (RUMC - formerly PMC)
Wholly owned by the RCSI and UCD, the University has been providing the highest quality medical education to internationally recognised standards since the institution’s inception in 1996. The core medical degree programme takes students to the RCSI or UCD in Dublin, Ireland for the pre-clinical years and then to RUMC and its Teaching Hospitals in and around Penang for their clinical training years prior to graduation. Graduates are awarded medical degrees of the National University of Ireland, which are recognised worldwide.
For centuries, physicians and scientists have thought of inflammation as the body's acute response to infection or injury, but in recent decades it's become clear that chronic inflammation drives pathologies as diverse as cancer, diabetes, and Alzheimer's disease. Controlling this aberrant inflammation, however, has proven difficult.
Conventional anti-inflammatory drugs work by antagonizing the body's pro-inflammatory hormones, but that approach also suppresses immunity, opening the patient to secondary infections. A newer strategy relies on recently discovered resolution mediators, compounds that the body makes naturally to resolve inflammatory responses without suppressing other parts of the immune system. Drugs targeting this process have shown immense potential to treat many of the world's most serious diseases, with fewer side effects than existing therapies.
On June 25–26, 2018, the New York Academy of Sciences hosted Resolution of Inflammation, Infection and Tissue Regeneration, a symposium featuring many of the top researchers in the rapidly developing field of resolution pharmacology. The meeting featured Professor Catherine Godson, UCD Professor of Molecular Medicine and Director, UCD Diabetes Complications Research Centre among the keynote speakers. In two days of oral presentations, a poster session, and an extensive panel discussion, speakers and attendees reviewed the biggest advances and challenges in resolution biology. The meeting covered the basic biology of inflammation and its resolution, studies on animal models of chronic and acute diseases, and clinical trials of promising new inflammation-resolving drugs.
You can find out more about the meeting from the e-Briefing which has been published by the New York Academy of Sciences.
Report by Alan Dove, New York Academy of Sciences. Reproduced and adapted with permission.
To mark 40 successful years of business in Ireland, Allergan introduced an annual €50,000 Innovation Award Programme in 2017. The Allergan Innovation Award Programme partnered with six Higher Education Institutions around Ireland, including University College Dublin (UCD), to recognise and support scholars who have excelled through innovative research in the field of life sciences.
The UCD Allergan Innovation Award will again feature as part of the 2018 UCD Conway Festival of Research & Innovation, a highlight in theUCD research calendar where there is specific emphasis on showcasing the innovative potential of current research projects being undertaken. A bursary of up to €8,000 will be awarded to the early career researcher(s) whose research shows greatest innovative potential.
UCD Allergan Innovation Award - Abstract Template
Cancer patients and their families were given a ‘behind-the-scenes’ look at the ongoing cancer research in the UCD Conway Institute and Systems Biology Ireland, as part of the fifth UCD Patient Voice in Cancer Research event on Friday, 21st September 2018.
The laboratory tours, which were led by senior scientists and their research teams, looked at a range of topics from how communication is broken in cancer cells to using biomarkers and risk calculators to predict the need for a biopsy in the diagnosis of prostate and breast cancer.
Academic lead for the initiative, Dr Amanda McCann, Associate Professor, UCD School of Medicine and Senior Fellow of UCD Conway Institute said,
“This event came about as a direct result of patients telling us that they want to know more about the research that is happening here in University College Dublin, see the research facilities and hear about the very exciting possibilities that may ultimately impact on the diagnosis and treatment of cancer patients in the future.”
Participants also had the opportunity to speak with representatives from patient advocacy and support groups; Movember Foundation, the Marie Keating Foundation, Purple House, OVACARE / SOCKS ISGO, ARC Cancer Support Centres, Lymphoedema Ireland, MAC Men against Cancer. Also exhibiting were MedEx Wellness, a community-based chronic illness rehabilitation programme located at Dublin City University; Theya Healthcare, who specialise in post-surgical lingerie, as well as EU funded industry-academia collaborative research projects for brain and colorectal cancer, Gliotrain & Colossus.
Tina O’Sullivan, a patient representative on the UCD Patient Voice in Cancer Research steering group responsible for coordinating the event exhibition said,
“We were delighted to welcome so many exhibitors to join this event, which was a fantastic opportunity for patients to hear first-hand how these organisations can support them in their cancer journey. The exhibitors also felt it was very informative as they were able to share information and ideas with fellow exhibitors which will ultimately be of great benefit to the patient”.
The UCD Patient Voice in Cancer Research is an initiative bringing together people living with cancer and their families with health care professionals, academic and clinical researchers; clinicians, patient advocates; funding agencies, policy makers and charity groups. It provides an open forum in which to identify the questions and needs that matter most to those living with a cancer diagnosis and those most likely to improve the relevance of cancer research.
While public and patient involvement (PPI) in research is a relatively new concept in Ireland, there are many examples of PPI in the United Kingdom and in Europe in the last ten years. Patient involvement in research can help to identify what research is important to fund, influence the way research is planned and how it will be carried out as well as improving the experience for people taking part in the research.
The UCD Patient Voice in Cancer Research steering group includes patients, scientists, health care professionals and patient advocacy groups. Patients and their families interested in hearing more about cancer research in University College Dublin and similar events under this initiative should email patientvoicecancer@ucd.ie or telephone (01) 716 6809.
Laboratory Tours (held on 21st September 2018)
Tour 1: "From cells to proteins; from proteins to networks: how do we find out how the cell communicates with the world and how communication is broken in cancer cells?" - Dr David Gomez
Tour 2: "Finding new treatments and biomarkers for breast and prostate cancer" – Dr Maria Prencipe and Dr Arman Rahman.
Tour 3: "Controlling the Spread of Cancer” - Associate Professor Margaret McGee
Tour 4: "Prostate cancer a 3-pronged approach: Prevention, Detection and Monitoring" - Associate Professor Antoinette Perry
Tour 5: "Tumour Cell Tweeting, communication between cancer cells using nanoparticles" - Associate Professor Amanda McCann
Tour 6: "Finding new therapeutic targets for malignant melanoma” — explore how we use a combination of cell biology and computer simulations to tackle skin cancer - Dr Jens Rauch
Tour 7: “Biomarkers and risk calculators to predict the need for a biopsy in the diagnosis of Prostate Cancer – Multidisciplinary approach” - Professor William Watson
“CFTR Corrector Triple-therapy shows great promise for patients with at least on copy of F508del, many of whom have no treatments available and severe progressive lung disease. Although the results of the Phase III trials are still awaited, there is great optimism that highly effective treatments for the most common type of genetic CF will be available to CF patients soon.”
“This is not a cure, but this gel could make skin stronger and could improve life expectancy as a result,”
said Debra Ireland’s head of research, Dr Sinead Hickey.
“It may also prevent wounds in the first place. If there are no wounds, then patients will suffer fewer infections, feel less pain, less itch and develop less skin cancer.”
Hickey also confirmed that a pharmaceutical company has taken over development of the gel, but has encouraged more people to continue donating to the charity to further more research.
“There are research projects similar to Prof Wang’s out there, waiting to be funded, which could bring us a step closer to a cure,”
she said.
“If charities like Debra Ireland aren’t investing in the early-stage research, we are never going to find the EB champion who can change the lives of this and future generations.”
Adapted from an original article in Silicon Republic.com https://www.siliconrepublic.com/machines/gene-gel-eb-butterfly-skin
Researchers at the UCD Charles Institute of Dermatology have developed a new gel that could one day drastically improve the quality of life of those living with the rare skin disease Epidermolysis Bullosa (known as EB).
Attendees of the last few Inspirefest events will have heard of the inspiring stories of those living with epidermolysis bullosa (EB). This is a rare skin disease caused by a fault in the gene that makes a vital protein responsible for keeping our layers of skin together.
Affecting approximately 300 people in Ireland, the condition seriously reduces a person’s quality of life, with painful blisters developing – both internally and externally – from the slightest bump.
Now, however, a team of researchers led by Prof Wenxin Wang has developed a gel-like treatment that could drastically improve the lives of those with EB as it helps to form functioning skin.
The gel works by inserting a functioning gene into skin cells and, so far, has been theoretically proven to work with one strand of the disease. This gives great hope for the team to carry out further studies to see if it will work on other forms of EB as well.
Another major positive about this treatment is that it does not involve skin grafting procedures, which can be very painful. The gene therapy research has been in the works for the past nine years with Prof Wenxin Wang between NUI Galway and UCD, with funding from EB charity Debra Ireland through public donations.
Postdoctoral researcher, Dr Ariane Watson has won the 2018 UCD Conway Festival gold medal for her work to identify cross-talk between epigenetic (chemical alternations to DNA) and cell signalling pathways in cancer. Dr Watson is part of a research team based in Systems Biology Ireland under the joint supervision of Conway Fellow, Professor Walter Kolch in UCD School of Medicine and Dr Colm Ryan, Assistant Professor in UCD School of Computer Science.
Ariane has been studying the patterns by which mutations in cancer genes occur; either two mutations always appearing together (co-occurrence) or when certain mutations never appear together (mutual exclusivity). This can indicate that there is an important biological relationship between the genes involved.
For example, co-occurring mutations often identify gene pairs whose mutations in combination result in a greater effect than each mutation alone. Mutually exclusive mutations can identify gene pairs that operate in common signalling pathways (e.g. BRAF and KRAS) or genes whose alteration in combination is lethal.
“I found statistically significant genetic interactions by analysing patterns of co-occurrence and mutual exclusivity between genetic alterations in 22 cancer studies from the Cancer Genome Atlas (TCGA), which can indicate meaningful biological relationships”, explains Ariane Watson.
Ariane was awarded the gold medal sponsored by Cruinn Diagnostics at the closing ceremony of the 2018 UCD Conway Festival of Research & Innovation. Professor William Gallagher, Director, UCD Conway Institute congratulated Ariane and nearly one hundred other early career researchers from across UCD Conway Institute who presented their research during the two day event.
“There have been many examples over the past two days within the poster and oral research presentations of high quality research findings that will undoubtedly become valuable additions to the international body of scientific knowledge; and may ultimately positively impact our society into the future”,
according to Professor Gallagher.
The judging panel for the 2018 UCD Conway Festival gold medal comprised plenary speakers, Alfred Wittinghofer, Emeritus Professor from the Max-Planck-Institute; Meinrad Gawaz, Professor & Medical Director of Cardiology and Cardiovascular Diseases, University of Tuebingen; Janet Iwasa, Research Assistant Professor, University of Utah and Professor William Gallagher, Director, UCD Conway Institute.
Ariane competed against five other early career researchers who were category winners in the moderated poster presentations. They are Matthew Whelan (PIs: Dr Tadhg Ó Cróinín, School of Biomolecular and Biomedical Science & Professor Jeremy Simpson, School of Biology and Environmental Science); Niamh Morgan (PI: Professor Jeremy Simpson, School of Biology and Environmental Science); Dr Fiona McCarthy (PI: Professor David Brayden, School of Veterinary Medicine); Siobhán Devlin (PI: Professor Paul McLoughlin, School of Medicine).
For the first time, the annual event also featured a session for early career researchers on public and patient involvement (PPI) in research, which included a keynote lecture from Dr Bettina Ryll, founder of the Melanoma Patient Network Europe.
During the PPI discussion forum, Marie Ennis-O’Connor, a digital strategist with extensive experience in patient involvement, facilitated a lively debate on the challenges and benefits of embedding PPI in research. The panel providing insight on the topic included Wendy Costello, Chair, iCAN Irish Children's Arthritis Network; Dr Avril Kennan, CEO, Medical Research Charities Group; Sinead Quinn (assoc. with Irish Sarcoma Group); Dr Emma Dorris, UCD; Dr Emmanuelle Vire, University College London and plenary speaker, Dr Bettina Ryll.
Also within this session, early career researcher and their patient mentors spoke about the experience of working together to improve the written communication of lay research abstracts. The original and revised versions of these lay abstracts formed part of the inaugural UCD Conway Engagement Badge poster competition. PhD students, Rebecca Ward (patient mentor: Gerard Eastwood) and Stephanie McKenna (patient mentor: Pat Fahey) won prizes for best poster presentation.
The 2018 UCD Allergan Innovation Award competition took place on the first day of the Festival. Dr Nicky Bertollo won first prize and a research bursary of €7000 to enable him to develop a new microneedle patch design to improve drug delivery through the skin. Microneedle patches (MNPs) have enormous potential for painless drug and vaccine delivery through the skin and for health monitoring. Dr Bertollo intends to use the bursary to carry out drug-coating and elution studies that will inform how his microneedle patch design can be brought to the next stage of development.
A second bursary prize of €1000 was presented to Barbara Hughes, a doctoral candidate working with Professor Sabine Koelle, UCD School of Medicine and Fellow, UCD Conway Institute. Barbara’s research aims to create new strategies for increasing fertility in couples as well as maintaining fertility in patients affected by gynaecological cancer. She intends to further develop a live cell imaging technology that will track the development of sperm inside the human fallopian tube.
Original article by UCD Conway Institute, reproduced with permission.
The effectiveness of early prophylactic hypothermia in improving long-term neurological outcomes in patients with severe traumatic brain injury (TBI) has been the subject of much debate for over thirty years. Not surprisingly given the challenges of conducting formalised studies in patients who experience sudden traumatic injury, many of the studies undertaken to date have failed to meet the standards necessary to draw definitive conclusions or have been limited by acknowledged potential publication bias.
The Prophylactic hypOthermia to Lessen traumatic bRain injury (POLAR) randomised controlled trial was designed by the Australian and New Zealand Intensive Care Society which included Prof Alistair Nichol, UCD Professor of Critical Care Medicine at St Vincent’s University Hospital while he was Associate Professor at the School of Public Health and Preventative Medicine at Monash University.
The Phase III trial took place across 6 countries over a ten year period recruiting 511 patients with severe traumatic brain injury from out-of-hospital and emergency department settings. The patients were randomised to early prophylactic hypothermia (33oC – 35oC) sustained for between 72 hours and up to 7 days if intracranial pressures were elevated with gradual rewarming or to controlled normothermia (37oC) for 7 days. The primary endpoint measure was favourable neurologic outcomes or independent living obtained by blinded assessors utilising a Extended Glasgow Outcome Scale (GOSE) score at 6 months after injury.
Among the 511 patients who were randomised, 500 provided ongoing consent and 466 completed the primary outcome evaluation. Favourable GOSE scores at 6 months occurred in 117 patients (48.8%) in the hypothermia group and 111 (49.1%) in the normothermia group. The study concluded that among patients with severe traumatic brain injury, early prophylactic hypothermia compared with normothermia did not improve neurological outcomes at 6 months. Hence these findings do not support the use of early prophylactic hypothermia for patients with severe traumatic brain injury.
Original Article
Cooper DJ, Nichol AD, Bailey M, Bernard S, Cameron PA, Pili-Floury S, Forbes A, Gantner D, Higgins AM, Huet O, Kasza J, Murray L, Newby L, Presneill JJ, Rashford S, Rosenfeld JV, Stephenson M, Vallance S, Varma D, Webb SAR, Trapani T, McArthur C; POLAR Trial Investigators and the ANZICS Clinical Trials Group.
JAMA. 2018 Oct 24. doi: 10.1001/jama.2018.17075.
An international research team exploring the development of recombinant human Alkaline Phosphatase (recAP) for the treatment of inflammatory diseases published data on the recently completed STOP-AKI Phase II study of recAP in the treatment of sepsis-associated Acute Kidney Injury (AKI). The results were published in the Journal of the American Medical Association (JAMA) and were presented at both the European Society of Intensive Care Medicine in Paris and at the American Society of Nephrology Kidney Week in San Diego.
Presenting the results of the randomised clinical study in Paris, Professor Peter Pickkers, MD PhD, Chair of Experimental Intensive Care Medicine, Radboud University Medical Center, and principal investigator of the STOP-AKI study said:
“Although the study did not meet its primary endpoint of short-term improvement in kidney function in the first 7 days, it did show long-term improvement in kidney function and very importantly a 40% relative reduction in mortality over placebo. In the absence of any drugs approved for this condition, these exciting clinical outcomes warrant further research to confirm these findings and to make this treatment available to patients.”
In addition, investigations at the institutions of Professor Mark D. Okusa and Professor Bruce Molitoris revealed more detail into recAP’s mode of action. Their research showed that protection from kidney injury is mediated by dephosphorylation by recAP of ATP to adenosine and activation of adenosine A2a receptors (A2aR).
Dr. Okusa, Professor of Medicine and Chief, Division of Nephrology and Director, Center for Immunity, Inflammation and Regenerative Medicine at University of Virginia, School of Medicine, and Dr. Molitoris, Professor of Medicine, former Director of Nephrology and the Indiana Center for Biological Microscopy at Indiana University noted:
“The mode of action appears to be an elegant, double effect; in the first instance recAP inactivates pro-inflammatory ATP, and the resulting formation of adenosine further reduces inflammation through the immunosuppressive adenosine A2a receptor pathway.”
Prof Patrick Murray, UCD Professor of Clinical Pharmacology who was a member of the original STOP-AKI Study design and steering committee expressed a hope that this study will lead to a Phase III trial to improve mortality in sepsis, an area of tremendous unmet need.
Erik van den Berg, CEO of Dutch biopharmaceutical company, AM-Pharma said:
“We are excited to share the clinical trial results in JAMA and scientific conferences. We are now preparing for the pivotal study to confirm the STOP-AKI study results, which could have a significant impact on patients with Acute Kidney Injury, for whom there is currently no treatment available.”
Previously, the US Food and Drug Administration granted Fast Track designation for recAP for treatment of sepsis-associated AKI. AKI involves inflammatory processes in the kidney which can lead to complete loss of renal function and is associated with high mortality rates.
Prof Murray highlighted the involvement of both academic and industry researchers in the collaboration and was pleased to note that the STOP-AKI trial had opened for recruitment in Dublin albeit shortly before the end of the recruitment period. It is hoped that there might be greater Irish participation in the Phase III trial through the Irish Critical-Care Clinical Trials Group led by Prof Alistair Nichol, UCD Professor of Critical Care Medicine.
About AM-Pharma www.am-pharma.com
AM‐Pharma is a biopharmaceutical company focused on the development of recAP (recombinant Human Alkaline Phosphatase) for treatment of Acute Kidney Injury (AKI), Ulcerative Colitis (UC), Necrotizing Enterocolitis (NEC) and Hypophosphatasia (HPP). Based on strong results from Phase II trials with bovine Alkaline Phosphatase in AKI and UC, AM‐Pharma has developed an innovative recombinant form of human Alkaline Phosphatase (recAP), and recently completed recruitment of 301 patients in the STOP-AKI adaptive Phase II trial for sepsis-associated AKI.
About Acute Kidney Injury
Acute Kidney Injury (AKI) involves inflammatory processes in the kidney which can lead to complete loss of renal function. Hospital‐acquired AKI affects annually around 3 million patients in Europe, the US and Japan, and is associated with mortality in roughly 700,000 patients. It occurs in as many as 4% of hospital admissions and 40% of critical care admissions. Depending on the severity and cause of renal injury, mortality ranges from 10% to as high as 70%. In the US alone, hospitals spend around $10 billion each year on managing this major medical problem. The most important causes of AKI are sepsis, cardiovascular surgery, exposure to nephrotoxic drugs and trauma. AKI patients that require dialysis have the worst prognosis. Currently the only treatment options are dialysis and supportive care. No drugs are approved to treat this condition. Typically, these patients are treated in Intensive Care Units, often with guidance by nephrologists.
About recAP
AM-Pharma’s therapeutic candidate, recAP (recombinant Alkaline Phosphatase), is a proprietary recombinant human AP constructed from two naturally occurring human isoforms of the AP enzyme, which is highly stable and active.
About STOP-AKI study
The trial, titled A Safety, Tolerability, Efficacy and QoL Study of Human recAP in the Treatment of Patients With SA-AKI (STOP-AKI), s an adaptive Phase II trial with two parts. In the first part, data from 120 patients were evaluated to select the most effective dose of recAP. In the second part, an additional 170 patients were recruited into two arms, receiving either the optimal dose of recAP identified initially, or placebo. The study recruited 301 patients in total, which makes it the largest interventional clinical study iwan AKI to date. The study was conducted in more than 50 intensive care units (ICU) in Western Europe and North America.
Saturday 13th October, University College Dublin
On Saturday 13th October 2018, the ultrasound team at UCD was delighted to welcome the British Medical Ultrasound Society back to Dublin for their fourth high profile study day. The day attracted 200 delegates from all over Ireland and the United Kingdom. UCD ultrasound lecturers Ms. Therese Herlihy (MSc programme director), Dr. Mary Moran, Mr. Kevin Cronin and Ms. Ann Fleming worked with the BMUS team to make this extremely well received study day happen. Experts from the UK and Ireland joined together to share their ultrasound knowledge and expertise.
The morning covered ultrasound topics common to all aspects of imaging such as ultrasound safety (Dr. Emma Chung, University of Leicester, UK), the importance of guidelines, documents and checklists (Mr. Peter Cantin, Derriford Hospital, UK) and reporting top tips and with delegate interaction (Mr. Colin Griffin, Royal Liverpool University Hospital & Mrs. Pamela Parker, BMUS Professional Development Office Hull and East Yorkshire Hospitals, UK). After morning coffee Mr. Peter Cantin and Mrs. Catherine Kirkpatrick (Lincoln County Hospital, UK) provided top tips for renal and gynae imaging. These sessions were followed by three former UCD MSc Ultrasound students who presented very interesting gynaecological ultrasound cases of a cervical ectopic pregnancy (Ms. Denise McGrath, Midlands Regional Hospital Mullingar), a struma ovarii (Ms. Bernice Dunne on behalf of Ms. Michele Keenan, Midlands Regional Hospital, Portlaoise) and an appendicitis found on transvaginal ultrasound (Ms. Maeve O Donnell, St. Vincent’s University Hospital, Dublin).
The afternoon sessions were divided into two streams, with one focusing on prenatal screening, Doppler ultrasound and multiple pregnancy and the second stream focusing on general medical ultrasound. In the general medical stream delegates listened to updates in imaging and top tips for biliary imaging (Mrs. Pamela Parker), chronic liver disease (Ms. Therese Herlihy, UCD), lower limb DVT assessment (Mr. Colin Griffin) and ultrasound of the head and neck (Mrs. Catherine Kirkpatrick). In the obstetrics stream Prof. Peter McParland, (UCD/National Maternity Hospital) provided delegates with an insight into developments in non-invasive prenatal testing, while Ms Cecelia Mulcahy (National Maternity Hospital, Dublin) shared her expert knowledge of Doppler techniques in antenatal scanning which was followed by Dr. Jennifer Walsh (UCD/National Maternity Hospital, Dublin) updating delegates on the clinical applications of Doppler in obstetric ultrasound. Dr. Stephen Carroll (National Maternity Hospital, Dublin) informed delegates about issues in ultrasound surveillance of twin pregnancies which was followed by Dr. Fionnuala Breathnach (RCSI/Rotunda Hospital, Dublin) communicating the results of the Multiple Pregnancy: Esprit Study Results and current national guidelines in Ireland.
Feedback from the study day was excellent from both faculty and delegates. The day sold out and highlighted a high demand for continuing ultrasound education. UCD and BMUS brought a renowned faculty of experts from the UK and Ireland to Dublin to provide this educational and inspiring packed programme and hopefully this wonderful sharing of knowledge and expertise will continue with another study day planned for September 2019.
The National University of Ireland held its annual Honorary Conferring Ceremony on the 11th of October 2018 in the Corrigan Hall of the Royal College of Physicians in Ireland. Four highly distinguished individuals were conferred with honorary degrees of the National University of Ireland at the Ceremony. The honorary graduates, all exceptional in their own fields are writer, producer & activist, Winne M. Li; Head Coach of the Irish rugby team, Joe Scmhidt; plastic surgeon, Professor Michael J Earley and Professor of English, Vera Kreilkamp. Speaking at the ceremony in the Royal College of Physicians in Ireland, the Chancellor of NUI Dr Maurice Manning congratulated the new graduates and commended them for their remarkable achievements.
Professor Cathal Kelly, Registrar of the Royal College of Surgeons in Ireland introduced Professor Michael J. Earley who was conferred with an Honorary Degree of Medicine. He referred to Professor Earley as “a distinguished surgeon and artist”, going on to say that his “career highlights the capacity of one individual to make a difference.” Professor Earley is currently Head of Global Standards of Operation Smile Ireland and UCD Clinical Professor. Having spoken to his colleagues, Professor Kelly said that he learned how Professor Earley is “driven by a commitment to quality of care”, seeing “these accolades and positions, not as reasons to celebrate, but as opportunities for improvement, in training and services.” He concluded by noting Professor Earley and his wife Finola’s involvement and commitment to charities such as the Cleft Lip and Palate Association of Ireland, the Chernobyl Children’s Project, The Healing Foundation (UK), The Neurofibromatosis Association of Ireland and the Christina Noble Foundation.
Professor of English, Vera Kreilkamp was conferred with the honorary Degree of Doctor of Literature. Speaking about Prof Kreilkamp’s contribution to Irish studies and literature, Professor Margaret Kelleher, University College Dublin spoke of her “outstanding work as a scholar, curator and educator and her key role in fostering influential public initiatives relating to culture, literature and the visual arts”. Commenting on her work, Prof Kelleher made reference to her co-creation of the 1996 art exhibition ‘America's Eye: Irish Painting from the Collection of Brian P. Burns’ which was shown in Boston College, Yale University, Washington DC and Dublin, saying that the works were “truly transformative in sharing knowledge and fostering appreciation of Irish visual culture and Irish material culture.” Prof Kelleher concluded by saluting Professor Kreilkamp’s “work as advocate and champion for the Irish visual and literary arts and as exemplary educator and scholar.”
Winne M. Li was introduced by Professor Emerita Patricia Coughlan, UCC who made reference to Li’s “insistence on openness (which) gives a powerful example of courage and straight thinking about this arena of extraordinary complexity and pain.” It is, she went on to say, “for Winnie Li’s singular, brave, and moving work towards such enlightenment that we duly honour her today.” Prof Coughlan noted the timeliness of the conferring of such an honour on Dr Li, who was conferred with an Honorary Doctor of Laws. She said that it was of particular signifigance in the context of the #MeToo movement and the “misogynist backlash we are now witnessing against women’s naming and challenging of endemic sexual bullying and coercion in all its forms, and of its enabling by patriarchy.”
Professor Pat Guiry of University College Dublin introduced honorary Doctor of Arts recipient Joe Schmidt, commenting that he is “lauded by a number of Ireland internationals as the brightest rugby mind they have ever come across in their careers”. Professor Guiry said that Schmidt is known “for analysing his opposition closely, for short, sharp training sessions, and for simple game strategies based on pressure, territory, intelligent defence with aggressive line speed, and rehearsed attacking plays.” He also paid tribute to Schmidt and his family’s dedication to raising public awareness of epilepsy, through work with Epilepsy Ireland. Prof Guiry concluded by telling of how Schmidt who was formerly an English teacher, quotes Aristotle to his players, saying "We are what we repeatedly do. Excellence is not an act, but a habit.” Dr Schmidt was honoured at the ceremony for his contribution to Irish life through rugby.
The conferring of Honorary Doctor of Laws on writer Michael J. Conry was postponed due to illness. NUI greatly looks forward to honouring Dr Conry’s contribution to Irish folklore and heritage at a later date.
Adapted from original article by National University of Ireland
An international collaboration jointly led by University College Dublin (UCD) and Monash University in Melbourne has found that mimicking the activity of molecules found naturally in the body may provide a new approach to treating vascular disease in diabetes.
Diabetes presents an enormous global health challenge. Currently 425 million people have diabetes and this is expected to rise to 750 million by 2025. It is estimated that 10% of our national healthcare budget relates to the management of diabetes and related complications.
People with diabetes have a high incidence of cardiovascular disease. A build-up of fat and immune cells [plaque] on blood vessels causes inflammation and plaque development. If a plaque ruptures, it can clog up a blood vessel and starve the brain of oxygen, resulting in stroke.
In healthy conditions, the body produces special messenger molecules that tightly control inflammation. In diseases such as diabetes, inflammation can become so vigorous that it overwhelms the activity of these messengers and rages out of control.
This research study carried out by Dr Eoin Brennan Lecturer/Assistant Professor in the UCD School of Medicine at the Conway Institute and investigators in Melbourne as part of an EU funded project took a radical approach of mimicking the activity of these messengers using a synthetic version of a molecule called lipoxin.
“I first worked with colleagues in the UCD School of Chemistry led by Professor Patrick Guiry to design a synthetic version of lipoxin called Benzo-LXA4. Then, I went to the laboratory of Professor Mark Cooper and Dr Phillip Kantharidis in Melbourne to look at the potential of using natural lipoxin and this synthetic mimic to treat vascular complications in diabetic animals. We were excited to find that not only did this decrease the amount of plaque in the blood vessels, it reversed established heart disease”, explained Dr Brennan.
Dr Brennan returned to UCD for the next stage of the project, which involved treating human carotid plaque tissue with these protective molecules to see if the findings in the laboratory were also relevant in the clinic. To do this, Ms Mary Barry and a team of vascular surgeons at St Vincent’s University Hospital, Dublin provided carotid plaque biopsy tissue after surgery to enable the UCD researchers to test the effects of the lipoxin drugs on patient tissue.
By taking the plaque tissue from human blood vessels and exposing it to lipoxin molecules in the laboratory, the research team found that inflammation was reduced. These results provide insights into the process of vascular damage seen in atherosclerosis, particularly in the diabetes setting, and identify lipoxins as a novel therapeutic for diabetic complications.
Importantly, the team showed that lipoxins could prevent the progression of atherosclerosis in animals with established atherosclerotic lesions. The study builds on earlier work by these scientists that showed these compounds reversed established diabetic kidney disease.
Co-senior author, Professor Catherine Godson, Director of the UCD Diabetes Complications Research Centre and Fellow of UCD Conway Institute said,
“This study highlights lipoxins as protective against diabetes-associated complications, such as accelerated atherosclerosis. It is important to recognise the novelty of this approach. The problems with anti-inflammatory drugs are well documented.
Here, we used an alternative, kinder and gentler approach than merely blocking inflammation. Instead, we have promoted its resolution by mimicking processes that keep us healthy. Based on these findings, we recently secured international support from the Juvenile Diabetes Research Foundation to look at how these lipoxin molecules interact with existing anti-diabetic therapies.”
Professor Mark Cooper, Head of the Diabetes Department in Monash University Central Clinical School and a world leading researcher in the field of diabetes and its complications said,
“In itself, this international collaboration has proved to be a truly fantastic example of translational medicine research; bringing together synthetic chemists with biomedical researchers and clinicians to move findings from laboratory models to ex-vivo tissue samples from patients.”
Dr Eoin Brennan is funded by an IRC ELEVATE Marie Curie Fellowship. The research is published in the current issue of the journal, Diabetes and is available online at - https://doi.org/10.2337/db17-1317; Lipoxins Protect against Inflammation in Diabetes-Associated Atherosclerosis.
Original Article:
Lipoxins Protect Against Inflammation in Diabetes-Associated Atherosclerosis
E. P. Brennan, M. Mohan, A. McClelland, M. de Gaetano, C. Tikellis, M. Marai, D. Crean, A. Dai, O. Beuscart, S. Derouiche, S.P. Gray, R. Pickering, M. Tan, M. Godson-Treacy, S. Sheehan, J.F. Dowdall, M. Barry, O. Belton, S.T. Ali-Shah, P.J. Guiry, K. Jandeleit-Dahm, M.E. Cooper, C. Godson and P. Kantharidis Diabetes 2018 Sep; db171317.https://doi.org/10.2337/db17-1317

Photo (Left to right): Dr Joe Gallagher, Mr Master Chisale and Dr Chris Watson
Master Chisale has just completed his MSc by research on childhood pneumonia in the community in Malawi. He spoke about what he has learned when undertaking this research in UCD.
I grew up in a rural area in the southern part of Malawi (Zomba) which is the old capital city of Malawi. I currently live in Mzuzu in the northern part of Malawi which is around 600km from my home area. I am a second born in a family of four children and I attended both primary and high school in the southern part of Malawi. My country, Malawi, has one of the lowest literacy rates in the world. Currently only around 60-70% of adults can read and write. Access to education is limited in Malawi particularly beyond primary school. Even in primary school there can be over 100 children in a class for one teacher. At the time I was selected to go to high school, I was the only person in the whole zone, which is comprised of around 10 government primary schools, to go to high school. In my whole clan, and the whole area I am from, I am the only one who has made it to University and it is exceptional for the whole region that I have now obtained an MSc.
I did my BSc in Biomedical Sciences at Mzuzu University from 2008 to 2012 and currently I am working with the Ministry of Health at Mzuzu Central Hospital, which is a tertiary referral hospital for the Northern Region. I am working as a medical laboratory scientist and lead the TB laboratory for the region. This position involves both on-bench technical sample analysis and management of the laboratory and staff. I am also head of research and publication at Mzuzu Central Hospital and I act as a mentor for students in Biomedical Sciences. I also teach at Mzuzu University in the Department of Biomedical Sciences and undertake practical sessions with students there.
I undertook an MSc by research in childhood pneumonia in UCD as I have been working for a number of years in respiratory disease, mostly focusing on TB. However, whereas TB receives much attention nationally and globally, I feel that childhood pneumonia is a neglected condition even though it is a very common condition in Malawi. Pneumonia remains the leading infectious cause of death among children under five, killing approximately 2,400 children a day worldwide. Most of its victims are less than 2 years old. I was interested to find out what effect new vaccinations provided in Malawi since 2012 (in particular pneumococcal vaccine) had on the cause of pneumonia in children. Also there are no definitive diagnostic tools to distinguish bacterial and viral infections quickly in childhood pneumonia, leading to high rates of antibiotic prescription. This is a major problem as antimicrobial resistance rises internationally. Finally most of the studies on childhood pneumonia have been undertaken in hospitals but in Malawi most children present and are treated in primary care alone, so we felt it was important to study pneumonia in this setting. My supervisors, Joe Gallagher and Chris Watson from the gHealth Research Group, obtained funding from the Bill and Melinda Gates Foundation to undertake a study of childhood pneumonia in primary care in Malawi. This allowed me the opportunity to undertake an MSc as part of this research project.
I had an opportunity to visit Ireland as part of my MSc and very much enjoyed my time in Ireland and at UCD (even if it was very cold!). It has been a great experience and I have formed a number of friendships with my colleagues and supervisors in UCD. We continue to work together and from a clinical aspect we have formed a link in Mzuzu Central Hospital with the Palms GP Surgery where Peter Harrington and Joe Gallagher are working. This project was supported by ESTHER Ireland and is now an ESTHER approved partnership which means that it is recognised that we work effectively and equitably together. This partnership is focused on improving the care of non-communicable diseases in Mzuzu. We are leading Malawi in developing innovative ways of providing care for these conditions in Africa and it is an exciting time for the hospital as we work together to develop initiatives in this area also.
However, primarily I like laboratory work (the most exciting moment of my MSc was when I got the first results of my swab PCR!) and I hope to focus on developing diagnostic tests for bacterial infection in childhood pneumonia in my PhD. I am currently seeking funding to undertake a PhD in this area and have formed links with a number of African countries through my work as an Ambassador for the American Society of Microbiology.
I very much appreciate the opportunity afforded by UCD in undertaking this MSc. I believe that Malawi, just like many African counties, has a lot of unanswered issues which can be best addressed if local research is prioritized. And I believe partnership with universities such as UCD can help us achieve this quickly and effectively. By working together we can build capacity in Malawi and achieve sustainable outcomes in science and health. Zikomo!
HSE INTERNSHIP APPLICATION, STAGE 1
Please be advised that the Stage 1 online application process for the 2019 medical intern intake will launch on the 19th October 2018 and the planned closing date of Stage 1 of the process is Tuesday 30th October 2018.
INTERN EMPLOYMENT ELIGIBILITY TEST (IEET, 2019)
Please note the IEET, Part 1 will be held on Friday, January 04 2019 & the IEET, Part 2 will be held on Friday, February 01 2019.
Full details regarding the IEET will be published in the HSE, Stage 1 internship guidebook released on 19th October, 2018.
More information : https://www.hse.ie/eng/staff/jobs/job-search/medical-dental/nchd/interns/
CRDI Online module
Expression of interest period: 15 Oct – 18 Nov 2018
This module introduces the concepts involved in the drug discovery and development process in the pharmaceutical industry and provides case studies of both small molecule and biotech molecule development from discovery to market. The module features perspectives from academia and industry, with input from university spin-offs, venture capitalists and patients.
Case Studies in Drug Discovery & Development, CRDI Online module
Free of charge for Postgraduate student, postdoctoral researcher, or member of staff in NUI Galway, RCSI, TCD, UCC, UCD, UL and affiliated hospitals
Further details at http://www.crdi.ie/education/courses/
A UCD Masterclass Programme was open to all Academic Track interns from around the country was held on Saturday, 8th September in the Catherine McAuley Education & Research Centre, Nelson Street, Dublin 7. This Masterclass is a formal teaching event facilitated by the UCD Intern Network and the UCD Clinical Research Centre supporting the Academic Track Intern Programme with the aim of fostering participants curiosity in pursuing a career as an academic clinician.
UCD Interns including Academic Track interns from UCD, UL & UCC attended the event as they embark on their Academic Track Programme which commenced on July 9th, 2018.
In attendance were Dr Evelyn Fennelly, UCD Academic track intern, Dr Sam Gray, UL Academic track intern, Dr Michael Hanrahan, UCC Academic track intern, Dr Louise Kelly, UCC Academic track intern, Dr Conor Keogh, UL Academic track intern, Dr Owen Killian, UCD Academic track intern, Dr Eithne Nic Ríogh, UCD Academic track intern, Dr Martin O Donnell, UCD Academic track intern and Dr Salim Sebaoui, UL Academic track intern including UCD Interns rotating through the Mater Misericordiae University Hospital & St Vincent’s University Hospital.
Topics and Speakers included:
Associate Professor Dermot Power, UCD Intern Network Coordinator would like to extend his thanks to all who participated in the event and to Professor Peter Doran, Director of the Clinical Research Centre for his valuable input and expertise in this subject area.
Details on the UCD Academic Track Programme can be found at here
The UCD Intern Network has four Academic Track Intern posts for 2018/2019. These UCD Academic Track Interns rotate through Medicine for the Elderly, Gastroenterology and Orthopaedics at the Mater Misericordiae University Hospital encompassing a three- month rotation for Clinical Research.
The following UCD Academic Track Interns were successfully allocated to these Academic Track Intern posts to complete the following research projects;
Dr Eithne Nic an Ríogh is completing a research project titled ‘Hepcare: Integrating Hepatitis C care for at risk patients’ with Prof Walter Cullen, Full Professor of Urban General Practice, School of Medicine, UCD and Dr Jack Lambert, Consultant Physician in Infectious Diseases, Mater Misericordiae University Hospital.
Dr Martin O Donnell is completing a research project titled ‘The Effects of Different Smoking Patterns in Pregnancy on Perinatal Outcomes’ with Professor Catherine Hayes, Associate Professor of Public Health, Institute of Population Health in Tallaght University Hospital, (TCD).
Dr Owen Killian is completing a research project titled ‘An investigation of the effects of transcranial neuromodulation on temporal processing abnormalities in Focal Dystonia’ with Professor Richard Reilly, Professor of Neural Engineering, Trinity College Institute for Neuroscience and St Vincent's University Hospital.
Dr Evelyn Fennelly is completing a research project titled ‘Role of miR-3613-3p and its target EGR-1 in the pathogenesis of ocular surface inflammation in primary Sjogren’s’ with Professor Conor Murphy, Professor of Ophthalmology, RCSI, St Stephen's Green.
Interns on the academic track have the benefit of:
Sat, 17 November 18 16:48
Dr Cliona McGovern has been selected and appointed for five years as an ethicist to the Federation of Royal Colleges of Physicians. Dr McGovern will be a member of the MRCP(UK) Scenario Editorial Committee (SEC). As a member of the SEC, she will advise on ethical matters relating to the use of scenarios, simulated patients, and the assessment of ethical principles and practices for the MRCP(UK) Part 2 Clinical Examinations. Dr McGovern will take an independent overview of the general proceedings and bring an external viewpoint on the development and quality assurance of the policies and processes of the MRCP examinations. This appointment will also have a role in assisting the Colleges in meeting their requirements as set out by the General Medical Council. As this appointment is to the Federation of Royal Colleges, Dr McGovern will be involved with colleagues in the Royal College of Physicians (London), the Royal College of Physicians of Edinburgh and the Royal College of Physicians and Surgeons of Glasgow.
The MRCP(UK) examinations are designed to test the skills, knowledge and behaviour of doctors in training. The MRCP(UK) Diploma is the knowledge-based assessment for core medical training in the UK. It has three parts; MRCP(UK) Part 1, MRCP(UK) Part 2 Written, MRCP(UK) Part 2 Clinical (Practical Assessment of Clinical Examination Skills [PACES]). Successful completion of the entire three-part examination is required before a doctor can start specialist internal medicine training in the UK. All of the MRCP(UK) and Speciality Certificate Examinations are approved by the General Medical Council as part of the UK postgraduate medical training programme.
The School is delighted to welcome applications for first time appointment, re-appointment or advancement within the 2019 UCD Medicine Clinical Pathway, the School's adjunct academic appointment scheme designed to recognise clinical staff who contribute to our programmes.
Applicants seeking advancement within the UCD Medicine Clinical Pathway should note that they will be required to demonstrate significant incremental performance across a number of the principal assessment criteria. The School’s Review Panel would ordinarily expect a minimum of three years between successive applications for promotion.
The UCD Medicine Clinical Pathway scheme is a formal University adjunct academic appointment and consistent with University procedures all appointments are for a period of up to five years although they may be extended by re-application.
| Stage | Indicative Time Frame |
| Open for Applications | 14th November 2018 - 5th January 2019 |
| Review by Section Leaders | 5th January 2019 - 15th February 2019 |
| Review Panel Assessment | TBC March 2019 |
| Submission to College | TBC April 2019 |
| Communication to Applicants | TBC April 2019/May 2019 |
| First Time Applications | 2019 UCD Medicine Clinical Pathway - First Time Appointments |
| Promotions | 2019 UCD Medicine Clinical Pathway - Promotions |
| Re-Appointments | 2019 UCD Medicine Clinical Pathway - Re-Appointments |
| Academic Section | Section Leader | Email Contact |
| Biomedical Sciences | Prof Paul McLoughlin | paul.mcloughlin@ucd.ie |
| General Practice | Prof Gerard Bury | gerard.bury@ucd.ie |
| Radiography & Diagnostic Imaging | Prof Louise Rainford | louise.rainford@ucd.ie |
| Medicine & Medical Specialties | Prof Yvonne O'Meara | yomeara@mater.ie |
| Surgery & Surgical Specialties | Prof Ronan Cahill | ronan.cahill@ucd.ie |
| Women's & Children's Health | Prof Fionnuala McAuliffe | fionnuala.mcauliffe@ucd.ie |
This adjunct academic appointment scheme recognises the contribution of our clinical faculty who lead or support both our teaching and our research programmes across our clinical training network. The School relies on clinicians within our affiliated teaching hospitals, acute, general and specialist hospitals and within primary care centres to deliver the clinical training component of our education programmes and to help drive our biomedical and clinical research programmes. We recognise that clinician engagement in University business is greatly facilitated by having a formal adjunct appointment. Hence in 2008, the School introduced the UCD Medicine Clinical Pathway scheme to provide formal university acknowledgement of these contributions to academic activities, recognising that many clinicians contribute strongly despite having no protected academic time.
Improving Critical Care Research for Patients and Family
Flu can spread easily from person to person and country to country. A Pandemic happens when a new kind of flu spreads across the world.
PREPARE is doing medical research in locations across Europe to help hospital doctors, GP's, and public health agencies respond to new outbreaks of flu. During a flu outbreak, research needs to be done quickly. This is where you can help!
We need to make sure this research is understandable and acceptable to patients and family. Building on the work of our project partners in Cardiff University who have set up a public panel, we are setting up a Dublin Public Panel who will ensure our research is relevant to local communities, advise on research information and design, and stay informed about ongoing critical care research.
The PREPARE group at the UCD School of Medicine are currently seeking members to join a public panel. This panel will meet 4-6 times a year to learn about and discuss epidemics and critical care research; advise on elements of the research process, and; improve the relevance and acceptability of critical care research design. The public panel will be of interest to individuals who'd like to learn more about epidemics and advise on the design of critical care research. The group are particularly interested in hearing from individuals who have experience (themselves/family member) of intensive care settings.
Sign up by emailing: prepare@ucd.ie
Telephone: 01 716 5823
Website: https://prepare.ucd.ie/
About PREPARE
PREPARE (Platform for European Preparedness Against (Re-)emerging Epidemics) is an EU funded network for harmonised large-scale clinical research studies on infectious diseases, prepared to rapidly respond to any severe ID outbreak, providing real-time evidence for clinical management of patients and for informing public health responses. Covering over 600 primary care sites and over 300 hospital sites in 27 European countries and other European countries and harbouring EU’s leading academic research groups on infectious diseases, PREPARE will transform Europe’s research response to future severe epidemics or pandemics. [more]
PREPARE is funded by the European Commission's FP7 Programme under grant number 602525. PREPARE has formally commenced its activities on 1 February 2014.
We are delighted to report that Dr Rhona Mahony, UCD Medicine alumna and Master of the National Maternity Hospital, Holles Street is being honoured by the University in the 2018 UCD Alumni Awards. A great supporter of our teaching programmes and of our student-led activities over many years, Dr Mahony (UCD MB BCh BAO 1994) has been selected in the category of Health Sciences.
Earlier this year, Dr Mahony was presented with an Honorary Fellowship of the UCD School of Medicine in recognition of her outstanding leadership in healthcare. In his citation at the 2018 UCD Medicine Conferring Dinner, then Dean of Medicine, Prof Patrick Murray noted that Rhona had become an inspiring role model for many medical students with her warm patient-focus and courageous pursuit of excellence in healthcare.
As the first female master since the foundation of the National Maternity hospital in 1894, Dr Rhona Mahony oversees one of Europe's largest Maternity hospitals, delivering almost 10,000 babies each year, a busy gynaecological unit and over 800 staff. A specialist in fatal foetal abnormalities and maternal medicine, she founded the National Maternity Foundation, which supports the work of the NMH. Dr Mahony has been published in a range of international academic journals. She is a Fellow of the RCOG UK, and of the RCPI in Ireland. In 2016 she was awarded an honorary Fellowship of the American College of O&G and an honorary Doctorate of Medicine from NUI for her contribution to women and infants’ health.
Introduced in 2014, the UCD Alumni Awards are designed to showcase the success and achievements of its graduates in their respective fields. Other UCD Medicine alumni who have been honoured by the University include Dr Patricia Scanlan (2014), Dr Patrick Bradley (2015), Dr Anne Merriman (2016) and Prof Garret FitzGerald (2017). The award will be presented to Dr Mahony at the 2019 UCD Alumni Awards event in UCD O'Reilly Hall on Friday 9th November 2018.
Thu, 1 November 18 14:40
The Faculty of Paediatrics at the Royal College of Physicians of Ireland have awarded that the inaugural Kathleen Lynn medal, in recognition of an outstanding contribution to Child Health, to Professor Karina Butler (UCD Medicine 1978), UCD Clinical Professor of Paediatrics, Consultant Paediatrician and Infectious Diseases Specialist at Our Lady's Children's Hospital Crumlin and Temple Street Children's University Hospital.
The Faculty of Paediatrics, in agreement with RCPI President Mary Horgan and RCPI Council, established the Kathleen Lynn Medal in 2018 to be awarded by the Faculty for exceptional service on behalf of children, especially in Ireland. It is the highest award in Ireland to recognise paediatricians that have been outstanding in their careers and in their contribution to paediatrics.
The medal was presented to Professor Butler at the Faculty of Paediatric Autumn conference on 12 October 2018.
Professor Karina Butler's professional life has been one of exceptional service on behalf of children. She is recognised internationally as an authority on Paediatric Infectious Diseases and a world expert in the field of Paediatric HIV/AIDS, particularly in the area of prevention of mother to child transmission. Cases of mother to child transmission of HIV are now a rarity in Ireland. The UCD Medicine alumna took up the position of Consultant Paediatrician with special interest in infectious diseases in Our Lady's Children's Hospital Crumlin in 1994. There she established the Rainbow Clinic National Centre for HIV Medicine in Children, where she works to this day. In addition to HIV infected children, the Rainbow clinic is the national referral centre for paediatric infectious diseases.
A Tireless Advocate for the Benefits of Vaccination
Karina was a leading force for the development of national guidelines for the management of congenital Hepatitis B, Hepatitis C, Herpes simplex, Syphyillis and Toxoplasmosis. She is a longstanding member and the current chair of the National Immunisation Advisory Committee and a tireless advocate for the benefits of vaccination for the children of Ireland.
Karina's efforts in the areas of prevention of congenital infection and childhood immunisation are all the more remarkable as they were achieved while she carried out her duties as the sole paediatric infectious dieases specialist in Ireland for over a decade.
Dr Kathleen Lynn (1874-1955) was the daughter of a Church of Ireland rector in Co. Mayo and her upbringing and education were that of a staunchly Protestant and Unionist family. She was deeply affected by the destitution that she witnessed as a child among the local population and as a result decided to become a doctor. She graduated from the Royal University of Ireland (now UCD) in1899 and she was elected a Fellow of the Royal College of Physicians in 1909.
She devoted most of her professional life in Dublin to caring for sick and malnourished children and with other colleagues established St. Ultan’s Hospital for infants. As well as treating sick and malnourished children, the hospital addressed the wider role of educating young mothers about breast-feeding and basic principles of hygiene and nutrition. Dr. Lynn was an ardent feminist and a patriot who supported the workers during the 1913 lockout and was Chief Medical Officer during the 1916 Easter Rising.
She also led the way for women working in Medicine in Ireland and St Ultan's was staffed mostly by female doctors. She did much to improve the lives of Irish children through medicine and education and we look forward to presenting this medal as our highest award to those making equally outstanding contributions to children's health.
Reproduced with kind permission from the Royal College of Physicians Ireland.
The first national arthritis research conference open to the public, medical professionals and academics took place today (Friday 2nd November 2018 in University College Dublin.
Involving patient expertise in the research that goes on to improve their quality of life seems obvious. However, traditionally, patients have not been involved in the decision making processes around health research.
The aim of this conference is to promote a more holistic approach to arthritis research and encourage public involvement in research. The entire conference will be accessible to the public and includes patient speakers and moderators, workshops designed by patients and workshops specifically for the public to demystify what research is, and how you can get involved.
"The ethos of UCD has always been embracing and inclusive, and we continue to expand this in all areas, including our research involvement and impact. We value the mutual benefit of engaging with wider society. Through initiatives such as this conference, we are are strengthening our holistic, strategic partnerships with public, community, educational institutions and professional organisations. In this way UCD can maximise our relevance and impact for our community and on society as a whole."
said Prof. Orla Feely, UCD Vice President for Research, Innovation and Impact
The conference is part of The Patient Voice in Arthritis Research initiative led by UCD Centre for Arthritis Research and supported by the Health Research Board of Ireland. Here, researchers are working together with patients, family members, carers and the interested public to improve research, health and quality of life for those living with arthritis.
Arthritis is the biggest cause of disability in Ireland and is a catch-all term for over 100 different conditions. It is a costly disease; both personally to those living with the disease, and to the economy.
Rheumatoid arthritis, which is due to a problem with the immune system, usually affects those of working age. About 75% of people diagnosed with rheumatoid arthritis are working at the time of diagnosis. The ability to work is affected in about half of these people within 5 years, with every third person diagnosed with rheumatoid arthritis becoming work disabled. About 22% of people will stop working entirely within 5 years due to their condition, and a further 18% will stop working due to a combination of arthritis and other factors such as depression.
Addressing the conference, Finian McGrath, TD. Minister of State for Disability Issues said,
"Arthritis is a condition that affects people of all ages. It is a common misconception that arthritis only affects older people. I understand that more than 1,200 children live with juvenile arthritis in Ireland and that one in five of arthritis patients are less than 55 years old. These statistics are striking. Today’s conference is about a collaborative approach to arthritis and rheumatic disease research. I believe in the power of collaboration and what can be achieved through such collaboration. I also wholeheartedly support the involvement of patients in research and in decision making in their treatment and am delighted that the conference is open to the public. It is hugely important that patients have a voice in research that has the potential to affect their day to day lives. A great example of such collaboration and inclusivity is UCD's Centre for Arthritis Research initiative ‘The Patient Voice in Arthritis Research’ which aims to ensure more public and patient involvement in arthritis research".
Ireland punches above its weight in terms of research into arthritis and other rheumatic diseases. There is a very active research community and have flourishing international partnerships. Significant investment has been focused on research by Arthritis Ireland, the Irish arthritis charity.
Commenting on The Patient Voice in Arthritis Research initiative, Dr Emma Dorris from UCD Centre for Arthritis Research said,
“Through The Patient Voice, we are working to reframe research to focus on the patient, rather than the disease. By working together, people with lived expertise of their disease, doctors, nurses, health professionals, scientists, economists, researchers and policy makers, will greatly increase the relevance and impact of research, and improve the quality of life for those living with arthritis, faster.”
The event took place on Friday, 02 November from 9.30am – 6pm in the George Moore auditorium, UCD O’Brien Centre for Science on the Belfield campus.
For further information
Dr. Emma Dorris, UCD Centre for Arthritis Research (Conference Organiser). emma.dorris@ucd.ie
Doctors may in the future be able to spare some prostate cancer patients the harsh effects of invasive treatments thanks to new research funded by the Irish Cancer Society. Using a new approach to identify and measure the aggressiveness of a patient’s prostate cancer, Irish-based researchers are developing a test which has so far proven to be more accurate than current clinical assessments.
Almost 3,500 men are diagnosed with prostate cancer each year in Ireland. However, many of these men will be diagnosed with low-grade, non-aggressive prostate cancer. In most of these situations, patients will have the option of undergoing ‘active surveillance’. This involves regular consultant visits and blood tests, and a biopsy every three years to check on the status of the cancer in lieu of immediate treatment.
For those men diagnosed with more aggressive prostate cancer, treatment can include radiotherapy or surgery, which can lead to side effects such as urinary and sexual problems. This research was led by Prof. William Watson, Full Professor of Cancer Biology, School of Medicine and Fellow, UCD Conway Institute. If verified through further research and introduced in clinics, the test could likely mean more men being spared such intense treatments where results would show them to be unnecessary.
Commenting on the research, which was recently published in the journal Medical Oncology, Prof Watson said:
“Using 156 Irish prostate cancer patient samples, we combined different biomarkers to see if they were more effective at measuring how aggressive the patient’s prostate cancer was. A biomarker is an indicator of the presence of diseases in our bodies, and includes changes in our DNA and proteins.
“We found that, when you combine the biomarkers measured in blood and tumour tissue you more accurately determine which patients have low-grade and aggressive disease. We also used a new mathematical formula to analyse the data, and it’s hoped this formula can be applied to other cancers to better understand how aggressive they are.”
The study involved researchers from UCD, TCD, RCSI and DCU and their affiliated hospitals, pooling their resources and expertise as part of the Prostate Cancer Research Consortium.
Dr Robert O’Connor, Head of Cancer Research at the Irish Cancer Society, added:
“This paper highlights vital work being undertaken by world class Irish cancer researchers to identify new ways to improve the diagnosis of cancer. This research is at an early stage and it will take more time and research until any potential benefits reach cancer patients. But it does show the building blocks required to lay the foundations to improve the quality of life of prostate cancer patients. The more we understand this disease, the better chance we have of stopping it in its tracks.”
“The Irish Cancer Society can only invest in vital research because of the public’s generous support. We currently fund more than 100 researchers across Ireland and have spent €25 million on life-saving cancer research since 2010. To continue doing this, we ask for the public’s continued support through their amazing fundraising efforts.”
The ‘Medical Oncology’ research paper Integrating biomarkers across omic platforms: an approach to improve stratification of patients with indolent and aggressive prostate cancer is available online: https://febs.onlinelibrary.wiley.com/doi/full/10.1002/1878-0261.12348
November marks Prostate Cancer Awareness Month and the Movember campaign. These findings are revealed as Movember campaign calls on the public to support men’s health. Since 2008, over 100,000 people have got involved and contributed to the Movember cause. Movember Ireland has funded over 30 prostate cancer initiatives, in partnership with the Irish Cancer Society, ranging from financial grants for patients and their families to ground-breaking research that has united the prostate cancer research community to improve outcomes and quality of life for the 1 in 7 Irish men who will get prostate cancer in their lifetime. Sign up now to support men’s health, visit Movember.com.
In UCD Conway Institute, our researchers are embracing the Movember actions of 'Grow, Move, Host'. The Conway Mo team have their funding page on https://moteam.co/conway-mo-team-2018.
Pictured at the UCD Conway Institute is Professor Stephen Pennington, UCD School of Medicine. (Nick Bradshaw, Fotonic).
The NovaUCD 2018 Innovation Award was presented to Professor Stephen Pennington, a global leader in proteomics research and innovation, by UCD President, Professor Andrew J. Deeks, at an event held at NovaUCD.
The Award was presented to the UCD Professor of Proteomics in recognition of his commitment and success in protein biomarker research, undertaken during the last 15-years at the UCD School of Medicine, and previously in the UK, and the conversion of this research into diagnostic tests for clinical use which can have a positive impact on the lives of patients worldwide.
Professor Pennington is the founder and Chief Scientific Officer of Atturos, a UCD spin-out company, which is developing a portfolio of novel multi-marker blood tests. Atturos’ first test, OCProDx, is a prostate cancer test which will help some men avoid unnecessary over treatment of their cancer. The company is planning to launch this test onto the market in 2020.
Every year over 1.2 million men globally receive a diagnosis of prostate cancer and the aim of Atturos’ test is to determine whether or not the cancer remains in the prostate or has spread beyond it. With this information, patients can make a more informed decision about their treatment, including the opportunity of monitoring the disease via active surveillance.
Professor Pennington is also the incoming President of the Human Proteome Organisation (HUPO), the international scientific organisation of over 1000 members representing and promoting proteomics, which is headquartered in Vancouver, Canada. He is the first researcher from an Irish University to be elected to this prestigious position.
Professor Andrew J. Deeks, UCD President said,
“I am delighted to present the NovaUCD 2018 Innovation Award to Professor Stephen Pennington. The Award recognises the quality and impact of his peer-reviewed research, over many years, and his commitment and continuing enthusiasm to convert the outputs of his protein biomarker research into diagnostic tests for clinical use.
Atturos, the company established by Professor Pennington, is currently developing a blood test to help men diagnosed with prostate cancer make more informed decisions about their treatment. This test can have significant benefit to patients worldwide and I wish him and the Atturos team every success with the launch of this test onto the global market.”
He added,
“This Award also recognises Steve as an innovation and entrepreneurial leader who combines excellence in teaching and research with a proven commitment to translating his research outcomes into commercial applications to impact the lives of people.”
Before moving to UCD in 2003 Professor Pennington was a Wellcome Trust lecturer at the University of Liverpool. There he became deeply involved in a new field of biochemistry research, now called proteomics, and co-authored the first review of this newly emerging field. While at Liverpool he also developed strong links with industry partners such as AB Sciex and Waters and was actively involved in technology licensing.
On moving to Ireland Professor Pennington helped to establish the University’s proteomics facility at the UCD Conway Institute. During the last 15-years he has been active in the implementation of collaborative proteomics projects, in particular clinical translational projects that align significant clinical needs to basic research.
In recent years this has been focused on the discovery and subsequent quantitative measurement of protein biomarker signatures, the latter using targeted proteomics strategies. It is this experience and expertise that lead to the establishment of Atturos.
On receiving the NovaUCD 2018 Innovation Award, Professor Stephen Pennington, said,
“It is a great honour to receive this prestigious Award and to follow in the footsteps of previous awardees. This Award reflects the valued guidance and input of many colleagues and collaborators over many years and the ‘can do’ attitude instilled in me by two remarkable ladies, my mother and grandmother. It also reflects the recent invaluable mentorship of Mike Feeney formerly of the IDA and Enterprise Ireland.”
He added,
“I am very excited about the potential of Atturos to make a significant impact in the new era of personalised medicine initially by helping men diagnosed prostate cancer make the life changing decisions they face. I would like to take this opportunity to acknowledge the huge support of Enterprise Ireland, NovaUCD, Agilent Technologies and MSC, amongst others, who have supported me and the Atturos team on our journey to date.”
He concluded,
“The Award also recognises the significant support and commitment of a large number of research colleagues, as well as current and past research students, who have worked closely with me over many years to help to develop our contribution to the proteomics research and innovation ecosystem at UCD, in Ireland and internationally.”
Professor Pennington is a named inventor on 4 priority patent filings and has also published over 90 scientific papers, edited and contributed to several books including editing one of the first books on proteomics that was translated into Chinese and Japanese. He is on the editorial board of several journals and regularly reviews manuscripts and grants for a number of organisations.
On an international level Professor Pennington has been the President of the British Society for Proteome Research since 2016 and in 2017 he was the lead organiser of the 16th Annual World Congress of the Human Proteome Organisation, held in the Convention Centre in Dublin. This Congress attracted 1500 delegates and included a gala dinner, in the Royal College of Physicians, at which former Vice-President Joe Biden was the guest of honour.
The NovaUCD Innovation Award was established in 2004 to highlight University College Dublin’s commitment to innovation. The Award is presented annually to an individual, company or organisation or group in recognition of excellence in innovation or of success achieved in the commercialisation of UCD research or other intellectual activity.
Article by Micéal Whelan, NovaUCD. Reproduced with permission.
A significant number of pregnant women in Ireland may be "secret smokers", leaving their baby at risk of being malnourished.
A new study of a group of mothers-to-be attending the Coombe Maternity Hospital found several were reluctant to disclose their habit. Researchers at the UCD Centre for Human Reproduction in the Coombe who questioned the 234 women presenting for antenatal care showed 15% admitted they were smokers. However, when they were given a breath carbon monoxide test another 10%, many well-educated, came clean on their persistent smoking, the 'European Journal of Obstetrics and Gynaecology and Reproductive Biology' reported.
Professor Michael Turner (UCD Professor of Obstetrics & Gynaecology and Director of the UCD Centre for Human Reproduction), who led the study, said that they were more likely than non-smokers to have a growth-restricted or malnourished baby - which increases the risk of an adverse pregnancy outcome such as stillbirth.
"Maternal smoking is arguably the most important modifiable risk factor for pregnancy in Ireland. The number of adults smoking in Ireland is declining slowly and most women quit spontaneously before they present for antenatal care. We found that 15% disclosed to the midwife at booking that they were persistent smokers. However, following a breath carbon monoxide test and a more detailed questioning from our research fellow, a further 10% disclosed their persistent smoking. Interestingly, we were surprised to find the non-disclosers were better educated."
Prof Turner said:
"We recommend therefore that all women presenting for antenatal care should have a breath carbon monoxide test to screen for persistent smoking."
He added:
"It is an inexpensive point-of-care test - less than the cost of a packet of cigarettes. If current smoking is confirmed, women should be offered a smoking cessation behavioural intervention and support. Most women will not engage during pregnancy itself with interventions but it should be offered again after delivery when nicotine replacement therapy can be safely offered."
If the test is positive, the women should have repeat ultrasound examinations in the third trimester to detect foetal growth restriction which may necessitate early delivery with induction or Caesarean section.
"We urge that all 19 maternity units screen for undisclosed maternal smoking. At present, only Letterkenny does so. It is an inexpensive way to improve the foetal outcomes and may have lifelong benefits."
The HSE said it provides a range of smoking cessation support services, some in the community and some in hospitals. Every cigarette smoked contains over 4,000 chemicals, so smoking when pregnant harms the unborn baby. Cigarettes can restrict the essential oxygen supply to the baby. As a result, their heart has to beat harder every time their mother smokes. It is possible to use nicotine replacement therapy during pregnancy. It is not recommended that pregnant women take 'stop smoking' tablets, such as Champix or Zyban.
Adapted from an original article by Eilish O’Regan, Irish Independent, 11th December 2018
The implications of high carbon monoxide levels in early pregnancy for neonatal outcomes.
Reynolds CME, Egan B, Kennedy RA, O'Malley E, Sheehan SR, Turner MJ.
Eur J Obstet Gynecol Reprod Biol. 2018 Nov 30;233:6-11. doi: 10.1016/j.ejogrb.2018.11.020. [Epub ahead of print]
After completing our move from Earlsfort Terrace in 2006, the School discovered approximately 1000 anatomy watercolour paintings which were taken at the old Richmond Hospital in Dublin. These highly detailed illustrations from 1850 - 1870 present a snapshot of a variety of medical conditions which were prevalent in the city at that time. The collection of images provide a fascinating insight into a very different era and includes hundreds of faces of Dublin’s citizens. The illustrations have recently been digitally scanned and catalogued by UCD Archives.

The images facilitate all manner of medical insight while also acting as a symbolic representation of hundreds of years of medical research, acting as a reminder to the wider medical community and general public that UCD, Dublin, and Ireland have always had an important part to play in Medicine.
The aim of this project was to have a team of medical students, supported by staff and faculty examine, research, study and review a selection of the water-colours. They developed poster style presentations which will form a permanent display at the Mater Misericordiae University Hospital, as well as a temporary exhibition in various locations across the UCD campus and at UCD community events, such as the UCD festival. The posters will also provide the basis for an electronic publication and the research undertaken will also be put forward for the UCD Student Medical Journal.
Eight School of Medicine students took part in the SPARC-funded project led by Mr Adam Tattersall and his Technology Enhanced Learning team called ‘The Brush and the Scalpel’. SPARC is an initiative of the UCD Career Development Centre and the project was supported by the Department of Surgery at the Mater Misericordiae University Hospital.
The eight students included David Burke, Camilla English, Jack Evans, Alan Hopkins, Emma Hughes, Joel Lee, Jia Wen Lok and Priscilla Pua. The students were supported by Mater Hospital and UCD staff: Ms Debbie Killeen, Prof Cahill, Mr Kevin Cronin, Prof Tim Lynch, Prof Padraic MacMathuna, Mr Dylan Murray, Mr Martin O'Donohoe and Ms Helena Rowley.
Also involved in the project were UCD Belfield staff including Adam Tattersall (SoM Technology Enhanced Learning Manager), Allison Kacperski (SoM Educational Technologist), Meadhbh Murphy (Archivist at UCD Library) and Rebecca Boyle (SPARC representative).
The project was funded by the SPARC (Supporting Partnerships And Realising Change) programme which enables UCD staff and students to work together on projects that make UCD and/or the surrounding community a better place to learn, work and live.